Massage Therapy for Neck Pain
/Massage therapy is being embraced by the medical community. This is because it is a non-pharmacological intervention that is simple to carry out, economical, and has very few side effects.
The Complex Clinical Picture of Neck Pain
Massage therapists are skilled in managing neck pain through a number of rehabilitation considerations including, but are not limited to:
• Manual Therapy (nerve mobilization, soft tissue massage, triggerpoint, IASTM)
• Education on Psychosocial Factors Such as Fear Avoidance
• Mindfulness-Based Stress Reduction
Assessing Neck Pain
Proper assessment help identify who is most likely to benefit from conservative treatments. Recent clinical guidelines published in the JOSPT suggest that patients with neck pain fall into 1 of 4 groups (Blandpied et al. 2017):
• neck pain with limited motion
• neck pain associated with whiplash
• headaches related to neck pain
• neck and nerve-related pain into the arm (also known as radicular pain).
Treating Neck Pain
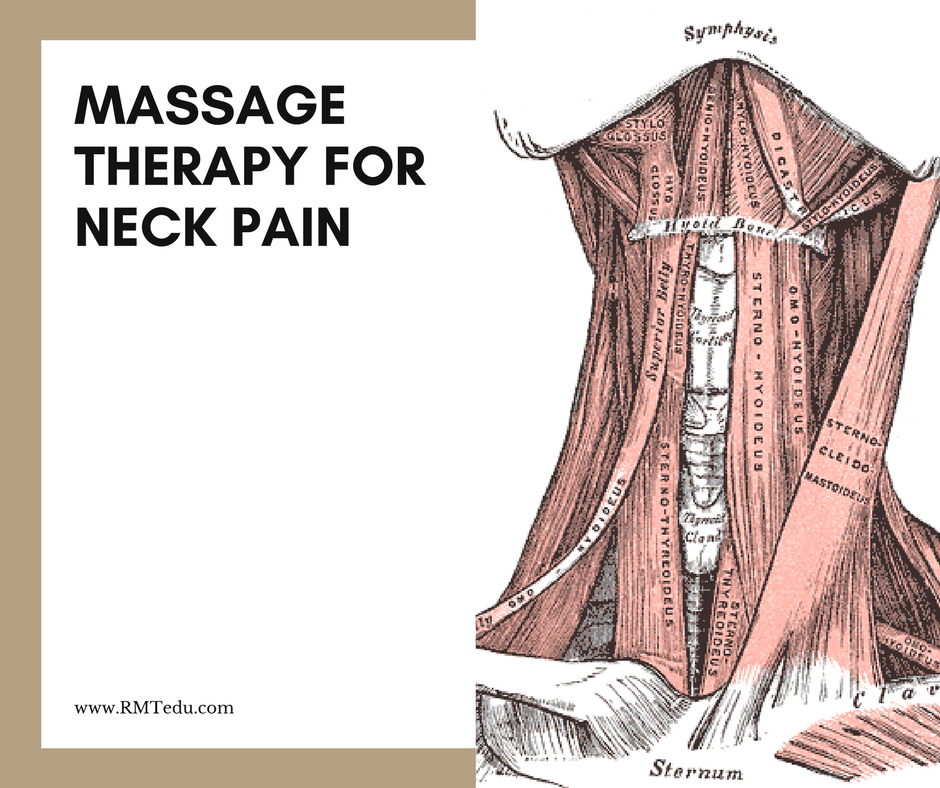
Once a proper assessment has been done, a massage therapy treatment plan can be implemented based on patient-specific assessment findings and patient tolerance. Structures to keep in mind while assessing and treating patients suffering from neck pain may include neurovascular structures and investing fascia of:
• Suboccipitals
• Upper Trapezius
• Splenius Cervicis
• Splenius Capitis
• Levator Scapula
• Rhomboids
• Occipitofrontalis
• Sternocleidomastoid
• Temporomandibular joint
• Scalene Muscle Group
More to Explore
Basson et al. (2017). The Effectiveness of Neural Mobilization for Neuro-Musculoskeletal Conditions: A Systematic Review and Meta-Analysis. J Orthop Sports Phys Ther.
https://www.ncbi.nlm.nih.gov/pubmed/28704626
Bier et al. (2018). Clinical Practice Guideline for Physical Therapy Assessment and Treatment in Patients With Nonspecific Neck Pain. Phys Ther.
https://www.ncbi.nlm.nih.gov/pubmed/29228289
Blanpied et al. (2017). Neck Pain: Revision 2017. J Orthop Sports Phys Ther
https://www.ncbi.nlm.nih.gov/pubmed/28666405
Bobos et al. (2018). Patient-Reported Outcome Measures Used for Neck Disorders: An Overview of Systematic Reviews. J Orthop Sports Phys Ther.
https://www.ncbi.nlm.nih.gov/pubmed/29932874
Brosseau et al. (2012). Ottawa Panel evidence-based clinical practice guidelineon therapeutic massage for neck pain. J Bodyw Mov Ther.
https://www.ncbi.nlm.nih.gov/pubmed/22703740
Busse et al. (2017). Guideline for opioid therapy and chronic noncancer pain. CMAJ.
https://www.ncbi.nlm.nih.gov/pubmed/28483845
Bussières et al. (2016). The Treatment of Neck Pain–Associated Disorders and Whiplash-Associated Disorders: A Clinical Practice Guideline. Journal of Manipulative and Physiological Therapeutics.
https://www.ncbi.nlm.nih.gov/pubmed/27836071
Chou et al. (2018). The Global Spine Care Initiative: applying evidence-based guidelines on the non-invasive management of back and neck pain to low- and middle-income communities. Eur Spine J.
https://www.ncbi.nlm.nih.gov/pubmed/29460009/
Childress & Becker (2016). Nonoperative Management of Cervical Radiculopathy. Am Fam Physician.
https://www.ncbi.nlm.nih.gov/pubmed/27175952
Cohen & Hooten. (2017). Advances in the diagnosis and management of neck pain. BMJ.
https://www.ncbi.nlm.nih.gov/pubmed/28807894
Cook et al. (2015). Randomized clinical trial assessing whether additional massage treatments for chronic neck pain improve 12- and 26-week outcomes. The Spine Journal.
https://www.ncbi.nlm.nih.gov/pubmed/26096474
Costello et al. (2016). The immediate effects of soft tissue mobilization versus therapeutic ultrasound for patients with neck and arm pain with evidence of neural mechanosensitivity: A randomized clinical trial. Journal of Manual & Manipulative Therapy.
https://www.ncbi.nlm.nih.gov/pubmed/27559283
De Meulemeester et al. (2017). Comparing Trigger Point Dry Needling and Manual Pressure Technique for the Management of Myofascial Neck/Shoulder Pain: A Randomized Clinical Trial. J Manipulative Physiol Ther.
https://www.ncbi.nlm.nih.gov/pubmed/28017188
Dewitte et al. (2016). Subjective and clinical assessment criteria suggestive for five clinical patterns discernible in nonspecific neck pain patients. A Delphi-survey of clinical experts. Man Ther.
https://www.ncbi.nlm.nih.gov/pubmed/27507590
Gerber et al. (2017). Beneficial Effects of Dry Needling for Treatment of Chronic Myofascial Pain Persist for 6 Weeks After Treatment Completion. PM R.
https://www.ncbi.nlm.nih.gov/pubmed/27297448
Gross et al. (2015). Manipulation and mobilisation for neck pain contrasted against an inactive control or another active treatment. Cochrane Database of Systematic Reviews.
https://www.ncbi.nlm.nih.gov/pubmed/26397370
Haller et al. (2016). Craniosacral Therapy for the Treatment of Chronic Neck Pain. The Clinical Journal of Pain. (OPEN ACCESS)
https://www.ncbi.nlm.nih.gov/pubmed/26340656
Kjaer et al. (2017). National clinical guidelines for non-surgical treatment of patients with recent onset neck pain or cervical radiculopathy. Eur Spine J.
https://www.ncbi.nlm.nih.gov/pubmed/28523381
Morikawa et al. (2017). Compression at Myofascial Trigger Point on Chronic Neck Pain Provides Pain Relief through the Prefrontal Cortex and Autonomic Nervous System: A Pilot Study. Front Neurosci. (OPEN ACCESS)
https://www.ncbi.nlm.nih.gov/pubmed/28442987
Nee et al. (2012). Neural tissue management provides immediate clinically relevant benefits without harmful effects for patients with nerve-related neck and arm pain: a randomised trial. Journal of Physiotherapy.
https://www.ncbi.nlm.nih.gov/pubmed/22341379
Sherman et al. (2014). Five-Week Outcomes From a Dosing Trial of Therapeutic Massage for Chronic Neck Pain. The Annals of Family Medicine.
https://www.ncbi.nlm.nih.gov/pubmed/24615306
Sherman et al. (2009). Randomized Trial of Therapeutic Massage for Chronic Neck Pain. The Clinical Journal of Pain.
https://www.ncbi.nlm.nih.gov/pubmed/19333174
Sutton et al. (2016). Is multimodal care effective for the management of patients with whiplash-associated disorders or neck pain and associated disorders? A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. The Spine Journal.
https://www.ncbi.nlm.nih.gov/pubmed/25014556
van der Velde et al. (2016). Which interventions are cost-effective for the management of whiplash-associated and neck pain-associated disorders? A systematic review of the health economic literature by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. The Spine Journal.
https://www.ncbi.nlm.nih.gov/pubmed/26631759
Walton & Elliott (2017). An Integrated Model of Chronic Whiplash-Associated Disorder. J Orthop Sports Phys Ther.
https://www.ncbi.nlm.nih.gov/pubmed/28622487
Wong et al. (2016). Are manual therapies, passive physical modalities, or acupuncture effective for the management of patients with whiplash-associated disorders or neck pain and associated disorders? an update of the bone and joint decade task force on neck pain and its associated disorders by the optima collaboration. The Spine Journal.
https://www.ncbi.nlm.nih.gov/pubmed/26707074