Massage Therapy For Frozen Shoulder
/Studies have demonstrated that conservative treatments may affect the progression of frozen shoulder.
Massage Therapy For Frozen Shoulder
A comprehensive treatment should incorporate a number of rehabilitation strategies based on patient-specific assessment findings including, but not limited to:
• Manual Therapy (nerve mobilization, soft tissue massage, triggerpoint, IASTM)
• Acupuncture (local, segmental and distal stimulation sites)
• Education on Psychosocial Factors (eg. BPS framework of pain, fear avoidance)
• Remedial Loading Programs (eg. static stretching, concentric, eccentric, isometric)
Patients benefit from the early diagnosis and proper treatment of frozen shoulder
This post is a brief look at related research, ideally it will serve as a starting point - providing massage therapists and researchers some points of considerations.
The development of a frozen shoulder is often classified as idiopathic (primary) or following shoulder surgery or trauma (secondary). Traditionally it has been taught that regardless of therapeutic intervention the affected shoulder will eventually improve or "thaw out".
This long held idea of complete resolution without treatment for frozen shoulder is unfounded. In most cases an understanding of the pathophysiology of frozen shoulder will lead to improved treatment outcomes, reduced pain and suffering associated with the condition (Wong et al. 2017).
The progression of the frozen shoulder is a complicated process, involving a cascade of molecular and cellular events.
Diabetic patients are more likely to develop frozen shoulder, but there are other comorbidities that exist. The storage of leukocytes and chronic inflammatory cells is thought to play a fundamental role in the development of frozen shoulder.
In this condition on going inflammation feeds into a cycle and is responsible for the upregulation of pro-inflammatory cytokine production, namely transforming growth factor beta (TGF-β). Which may be further perpetuated by sympathetic dominance of autonomic balance, and neuro-immune activation (Pietrzak 2016).
Impacting inflammation with manual therapy and gentle stretching
The responses to massage therapy are multifactorial - physiological and psychological factors interplay in a complex manner. A biopsychosocial framework is a practical approach for investigating the complex interplay between massage therapy and the experience of pain.
Additionally, based on available evidence gentle mobilization serves to interrupt the sequelae of pathological healing. This is most likely not in a single unified response, but as a collection of interconnected adaptive responses within the nervous system and soft tissue structures.
Attenuating Tissue Levels of TGF-β1 - As a therapeutic intervention massage therapy has the potential to attenuate TGF-β1 induced fibroblast to myofibroblast transformation. Recent studies have looked at the effect of modeled massage therapy and mechanical stretching on tissue levels of TGF-β1 (Bove et al. 2016). In this study it was demonstrated that mechanical stretching has the potential to attenuate tissue levels of TGF-β1 and the development of fibrosis. This is potentially impactful in the treatment of frozen shoulder because TGF-β1 plays a key role in tissue remodeling and fibrosis.
Impacting Inflammation - Persistent inflammation has the potential to interfere with the remodeling of tissue. Modeled experiments have demonstrated the impact of stretching on inflammation-regulation mechanisms within connective tissue (Berrueta et al. 2016). Additionally, studies have suggested that the application of massage induces a phenotype change, prompting the transition of M1 macrophages (pro-inflammatory) into the M2 macrophages (anti-inflammatory) (Waters-Banker et al. 2014).
Postoperative frozen shoulder is a serious complication after shoulder surgery, with an incidence of 11% (Koorevaar et al. 2017). If clinically translatable, prophylactic massage treatments could make a large impact for post-operative patients. The hypothesis that massage therapy effects the progression of post-operative frozen shoulder by inhibiting inflammatory processes and affecting the development of fibrosis by mediating differential cytokine production warrants further research.
The complex clinical picture of frozen shoulder
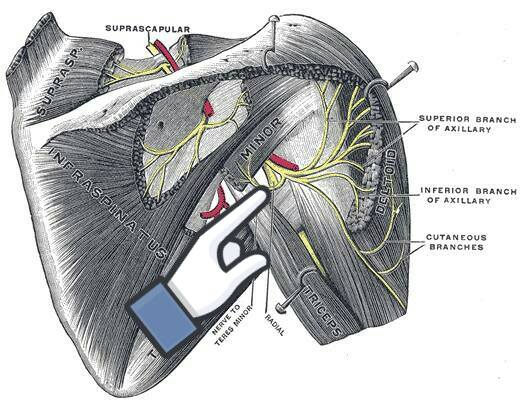
A treatment plan should be implemented based on patient-specific assessment findings and patient tolerance. I often treat this area while passively moving the arm through a wide range of motion. Gently stretching the muscles, neurovascular structures and investing fascia of:
• the rotator cuff
• teres major
• triceps brachii
• pectoral muscle group
• serratus anterior
• coricobracialis
• latissimus dorsi
• deltoids
More to Explore
Alsubheen et al. (2019). Effectiveness of Nonsurgical Interventions for Managing Adhesive Capsulitis in Patients With Diabetes: A Systematic Review. Arch Phys Med Rehabil.
https://www.ncbi.nlm.nih.gov/pubmed/30268804
Berrueta et al. (2016). Stretching Impacts Inflammation Resolution in Connective Tissue. Journal of Cellular Physiology.
https://www.ncbi.nlm.nih.gov/pubmed/26588184
Bove et al. (2016). Manual therapy as an effective treatment for fibrosis in a rat model of upper extremity overuse injury. Journal of the Neurological Sciences.
http://www.ncbi.nlm.nih.gov/pubmed/26810536
Chapman et al. (2016). Skeletal muscle fibroblasts in health and disease. Differentiation.
https://www.ncbi.nlm.nih.gov/pubmed/27282924
Clewley et al. (2014). Trigger point dry needling as an adjunct treatment for a patient with adhesive capsulitis of the shoulder. J Orthop Sports Phys Ther.
https://www.ncbi.nlm.nih.gov/pubmed/24261931
Cucchi et al. (2017). Risk Factors for Shoulder Stiffness: Current Concepts. Joints.
https://www.ncbi.nlm.nih.gov/pubmed/29270559
D'Orsi et al. (2012). Treatment of adhesive capsulitis: a review. Muscles Ligaments Tendons J.
https://www.ncbi.nlm.nih.gov/pubmed/23738277
Eljabu et al. (2016). Prognostic factors and therapeutic options for treatment of frozen shoulder: a systematic review. Arch Orthop Trauma Surg.
https://www.ncbi.nlm.nih.gov/pubmed/26476720
Farrell, K., & Lampe, K. (2017). Addressing neurodynamic irritability in a patient with adhesive capsulitis: a case report. J Man Manip Ther.
https://www.ncbi.nlm.nih.gov/pubmed/28855792/
Freitas et al. (2017). Can chronic stretching change the muscle-tendon mechanical properties? A review. Scand J Med Sci Sports.
https://www.ncbi.nlm.nih.gov/pubmed/28801950
Gigliotti et al. (2017). Fibrosis, low vascularity, and fewer slow fibers after rotator-cuff injury. Muscle Nerve.
https://www.ncbi.nlm.nih.gov/pubmed/2757128
Hawk et al. (2017). Systematic Review of Nondrug, Nonsurgical Treatment of Shoulder Conditions. J Manipulative Physiol Ther.
https://www.ncbi.nlm.nih.gov/pubmed/28554433
Horst et al. (2017). Activity- vs. structural-oriented treatment approach for frozen shoulder: a randomized controlled trial. Clin Rehabil.
https://www.ncbi.nlm.nih.gov/pubmed/28081633
Itoi et al. (2016). Shoulder Stiffness: Current Concepts and Concerns. Arthroscopy.
https://www.ncbi.nlm.nih.gov/pubmed/27180923
Johnson et al. (2007). The effect of anterior versus posterior glide joint mobilization on external rotation range of motion in patients with shoulder adhesive capsulitis. J Orthop Sports Phys Ther.
https://www.ncbi.nlm.nih.gov/pubmed/17416123
Koorevaar et al. (2017). Incidence and prognostic factors for postoperative frozen shoulder after shoulder surgery: a prospective cohort study. Arch Orthop Trauma Surg.
https://www.ncbi.nlm.nih.gov/pubmed/28132086
Le et al. (2017). Adhesive capsulitis of the shoulder: review of pathophysiology and current clinical treatments. Shoulder Elbow.
https://www.ncbi.nlm.nih.gov/pubmed/28405218
Lewis, J. (2015). Frozen shoulder contracture syndrome - Aetiology, diagnosis and management. Man Ther.
https://www.ncbi.nlm.nih.gov/pubmed/25107826
Page et al. (2014). Manual therapy and exercise for adhesive capsulitis (frozen shoulder). Cochrane Database of Systematic Reviews Reviews.
https://www.ncbi.nlm.nih.gov/pubmed/25157702
Page, P., & Labbe, A. (2010). Adhesive capsulitis: use the evidence to integrate your interventions. N Am J Sports Phys Ther.
https://www.ncbi.nlm.nih.gov/pubmed/21655385
Pietrzak, M. (2016). Adhesive capsulitis: An age related symptom of metabolic syndrome and chronic low-grade inflammation? Med Hypotheses.
https://www.ncbi.nlm.nih.gov/pubmed/26880627
Rawat et al. (2016). Effect of rotator cuff strengthening as an adjunct to standard care in subjects with adhesive capsulitis: A randomized controlled trial. J Hand Ther.
https://www.ncbi.nlm.nih.gov/pubmed/27884497
Ryan et al. (2016). The pathophysiology associated with primary (idiopathic) frozen shoulder: A systematic review. BMC Musculoskeletal Disorders.
https://www.ncbi.nlm.nih.gov/pubmed/27527912
Sawyer et al. (2018). Use of Pain Neuroscience Education, Tactile Discrimination, and Graded Motor Imagery in an Individual With Frozen Shoulder. J Orthop Sports Phys Ther.
https://www.ncbi.nlm.nih.gov/pubmed/29257926/
Schröder et al. (2017). Immediate Pain Relief in Adhesive Capsulitis by Acupuncture-A Randomized Controlled Double-Blinded Study. Pain Med.
https://www.ncbi.nlm.nih.gov/pubmed/28371868
Stecco et al. (2016). Fascial Disorders: Implications for Treatment. Pm&r.
https://www.ncbi.nlm.nih.gov/pubmed/26079868
Struyf, F., & Meeus, M. (2014). Current evidence on physical therapy in patients with adhesive capsulitis: what are we missing? Clin Rheumatol.
https://www.ncbi.nlm.nih.gov/pubmed/24374758
Waters-Banker et al. (2014). Investigating the Mechanisms of Massage Efficacy: The Role of Mechanical Immunomodulation. Journal of Athletic Training.
https://www.ncbi.nlm.nih.gov/pubmed/24641083
Whelton, C., & Peach, C.A. (2018). Review of diabetic frozen shoulder. Eur J Orthop Surg Traumatol.
https://www.ncbi.nlm.nih.gov/pubmed/29094212
Wong et al. (2017). Natural history of frozen shoulder: fact or fiction? A systematic review. Physiotherapy.
https://www.ncbi.nlm.nih.gov/pubmed/27641499
Yang et al. (2017). Prevalence and risk factors of adhesive capsulitis of the shoulder after breast cancer treatment. Support Care Cancer.
https://www.ncbi.nlm.nih.gov/pubmed/27942856