Musculoskeletal Pain and Treatment-Related Plasticity
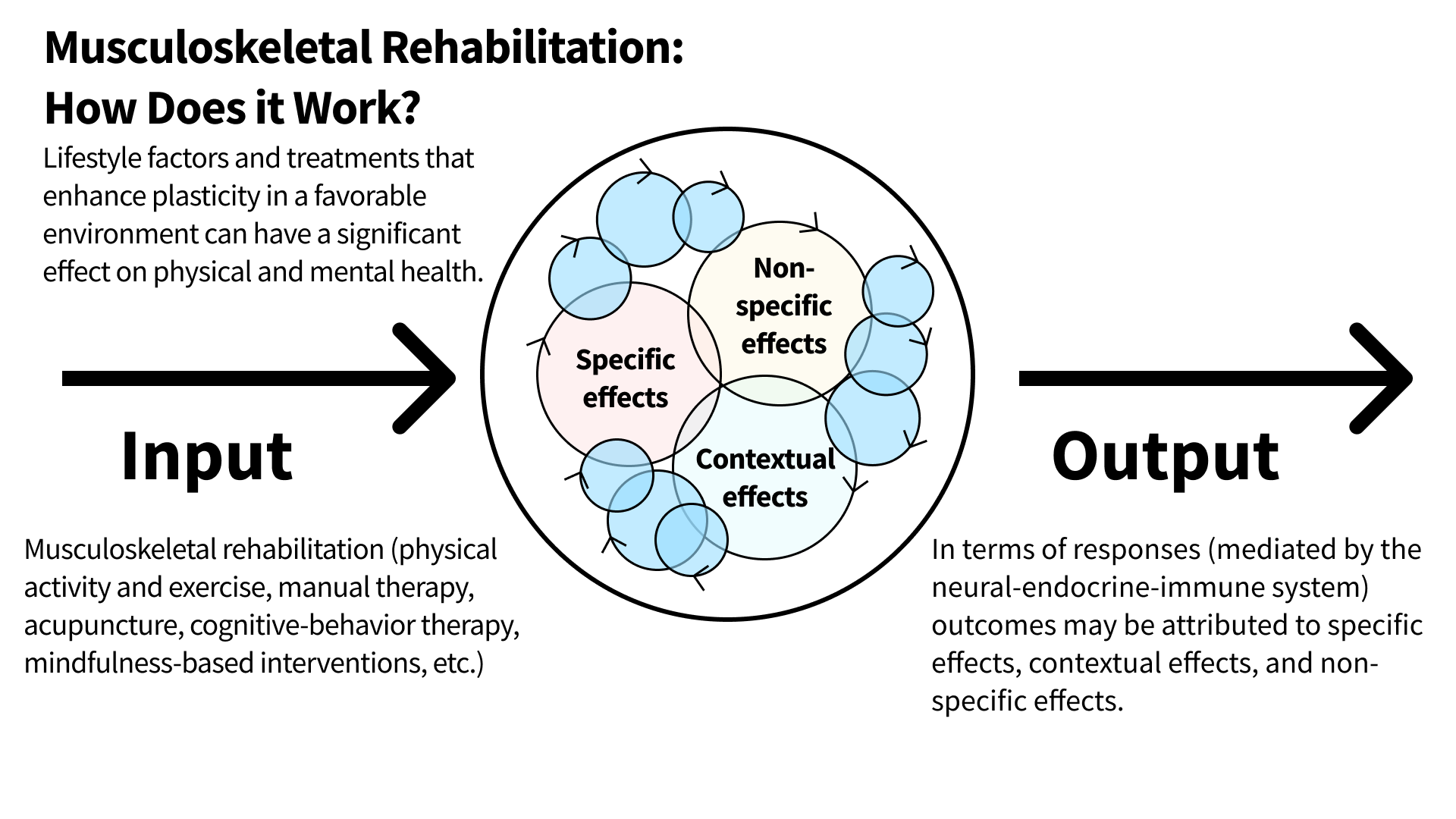
/Lifestyle factors and treatments that enhance plasticity in a favorable environment can have a significant effect on physical and mental health. These outcomes may be attributed to specific effects (physiological, neurobiological), contextual effects (patient-therapist relationship, set and setting), and non-specific effects (natural history, regression toward the mean).
Musculoskeletal Pain and Treatment-Related Plasticity
Treatments for musculoskeletal pain often have similar outcomes. One underlying concept with relevance to musculoskeletal rehabilitation (physical activity and exercise, manual therapy, acupuncture, cognitive-behavior therapy, mindfulness-based interventions, etc.) is plasticity.
Plasticity is the ability to modify activity and structure at neural and/or behavioral levels. Central to the concept of plasticity is that people are constantly changing in response to their internal and external environment. This dynamic bi-directional relationship between subjects and their environment is mediated by a whole-body neuro-endocrine-immune response.
Lifestyle factors and treatments that enhance plasticity (physiological, neurobiological, behavioral, etc.) in a favorable environment can have a significant effect on physical and mental health by nudging from a pathological state toward a healthy state.
Lifestyle factors and treatments that enhance plasticity (physiological, neurobiological, behavioral, etc.) in a favorable environment can have a significant effect on physical and mental health by nudging from a pathological state toward a healthy state.
Image From - Branchi, I. (2022). Plasticity in mental health: A network theory. Neuroscience and biobehavioral reviews, 138, 104691. https://doi.org/10.1016/j.neubiorev.2022.104691
References & Sources
Bernard, C., Zavoriti, A., Pucelle, Q., Chazaud, B., & Gondin, J. (2022). Role of macrophages during skeletal muscle regeneration and hypertrophy-Implications for immunomodulatory strategies. Physiological reports, 10(19), e15480. https://doi.org/10.14814/phy2.15480
Boendermaker, B., Buechler, R., Michels, L., Nijs, J., Coppieters, I., & Hotz-Boendermaker, S. (2022). Adaptive changes in sensorimotor processing in patients with acute low back pain. Scientific reports, 12(1), 21741. https://doi.org/10.1038/s41598-022-26174-2
Branchi, I. (2022). Plasticity in mental health: A network theory. Neuroscience and biobehavioral reviews, 138, 104691. https://doi.org/10.1016/j.neubiorev.2022.104691
Cashin, A. G., McAuley, J. H., Lamb, S. E., & Lee, H. (2021). Disentangling contextual effects from musculoskeletal treatments. Osteoarthritis and cartilage, 29(3), 297–299. https://doi.org/10.1016/j.joca.2020.12.011
Chapman, C. R., Tuckett, R. P., & Song, C. W. (2008). Pain and stress in a systems perspective: reciprocal neural, endocrine, and immune interactions. The journal of pain, 9(2), 122–145. https://doi.org/10.1016/j.jpain.2007.09.006
Cui, X., Liu, K., Gao, X., & Zhu, B. (2022). Advancing the Understanding of Acupoint Sensitization and Plasticity Through Cutaneous C-Nociceptors. Frontiers in neuroscience, 16, 822436. https://doi.org/10.3389/fnins.2022.822436
Diniz, C. R. A. F., & Crestani, A. P. (2022). The times they are a-changin': a proposal on how brain flexibility goes beyond the obvious to include the concepts of "upward" and "downward" to neuroplasticity. Molecular psychiatry, 10.1038/s41380-022-01931-x. Advance online publication. https://doi.org/10.1038/s41380-022-01931-x
Egan, B., & Sharples, A. P. (2022). Molecular Responses to Acute Exercise and Their Relevance for Adaptations in Skeletal Muscle to Exercise Training. Physiological reviews, 10.1152/physrev.00054.2021. Advance online publication. https://doi.org/10.1152/physrev.00054.2021
Fitzcharles, M. A., Cohen, S. P., Clauw, D. J., Littlejohn, G., Usui, C., & Häuser, W. (2021). Nociplastic pain: towards an understanding of prevalent pain conditions. Lancet (London, England), 397(10289), 2098–2110. https://doi.org/10.1016/S0140-6736(21)00392-5
Gallagher, S., & Barbe, M. (2022). Musculoskeletal Disorders: The Fatigue Failure Mechanism. Wiley.
Hettinger, Z. R., Wen, Y., Peck, B. D., Hamagata, K., Confides, A. L., Van Pelt, D. W., Harrison, D. A., Miller, B. F., Butterfield, T. A., & Dupont-Versteegden, E. E. (2022). Mechanotherapy Reprograms Aged Muscle Stromal Cells to Remodel the Extracellular Matrix during Recovery from Disuse. Function (Oxford, England), 3(3), zqac015. https://doi.org/10.1093/function/zqac015
Hodges, P. W., Barbe, M. F., Loggia, M. L., Nijs, J., & Stone, L. S. (2019). Diverse Role of Biological Plasticity in Low Back Pain and Its Impact on Sensorimotor Control of the Spine. The Journal of orthopaedic and sports physical therapy, 49(6), 389–401. https://doi.org/10.2519/jospt.2019.8716
Huston, P. (2022). A Sedentary and Unhealthy Lifestyle Fuels Chronic Disease Progression by Changing Interstitial Cell Behaviour: A Network Analysis. Frontiers in physiology, 13, 904107. https://doi.org/10.3389/fphys.2022.904107
Isenburg, K., Mawla, I., Loggia, M. L., Ellingsen, D. M., Protsenko, E., Kowalski, M. H., Swensen, D., O'Dwyer-Swensen, D., Edwards, R. R., Napadow, V., & Kettner, N. (2021). Increased Salience Network Connectivity Following Manual Therapy is Associated with Reduced Pain in Chronic Low Back Pain Patients. The journal of pain, 22(5), 545–555. https://doi.org/10.1016/j.jpain.2020.11.007
Jain, A., Hakim, S., & Woolf, C. J. (2020). Unraveling the Plastic Peripheral Neuroimmune Interactome. Journal of immunology (Baltimore, Md. : 1950), 204(2), 257–263. https://doi.org/10.4049/jimmunol.1900818
Laukkonen, R. E., & Slagter, H. A. (2021). From many to (n)one: Meditation and the plasticity of the predictive mind. Neuroscience and biobehavioral reviews, 128, 199–217. https://doi.org/10.1016/j.neubiorev.2021.06.021
Li, Q., Zhao, W., & Kendrick, K. M. (2022). Affective touch in the context of development, oxytocin signaling, and autism. Frontiers in psychology, 13, 967791. https://doi.org/10.3389/fpsyg.2022.967791
Ma, X., Chen, W., Yang, N. N., Wang, L., Hao, X. W., Tan, C. X., Li, H. P., & Liu, C. Z. (2022). Potential mechanisms of acupuncture for neuropathic pain based on somatosensory system. Frontiers in neuroscience, 16, 940343. https://doi.org/10.3389/fnins.2022.940343
Maeda, Y., Kim, H., Kettner, N., Kim, J., Cina, S., Malatesta, C., Gerber, J., McManus, C., Ong-Sutherland, R., Mezzacappa, P., Libby, A., Mawla, I., Morse, L. R., Kaptchuk, T. J., Audette, J., & Napadow, V. (2017). Rewiring the primary somatosensory cortex in carpal tunnel syndrome with acupuncture. Brain: a journal of neurology, 140(4), 914–927. https://doi.org/10.1093/brain/awx015
McParlin, Z., Cerritelli, F., Rossettini, G., Friston, K. J., & Esteves, J. E. (2022). Therapeutic Alliance as Active Inference: The Role of Therapeutic Touch and Biobehavioural Synchrony in Musculoskeletal Care. Frontiers in behavioral neuroscience, 16, 897247. https://doi.org/10.3389/fnbeh.2022.897247
Miller, M., Albarracin, M., Pitliya, R. J., Kiefer, A., Mago, J., Gorman, C., … Ramstead, M. J. (2022). Resilience and Active Inference. https://doi.org/10.31234/osf.io/vehq2
Salgado, A., Takemoto, M. H., de Souza, C., Salm, D. C., da Rosa, D., Cardoso, G. C., Ludtke, D. D., Soares, S., Ferreira, J. K., Dutra, A. R., Szeremeta, Y. C., Mazzardo, G., Mayra, J., Sheffer, D., Caumo, W., Bittencourt, E. B., Schleip, R., Latini, A., Bobinski, F., & Martins, D. F. (2022). Gentle Touch Therapy, Pain Relief and Neuroplasticity at Baseline in Fibromyalgia Syndrome: A Randomized, Multicenter Trial with Six-Month Follow-Up. Journal of clinical medicine, 11(16), 4898. https://doi.org/10.3390/jcm11164898
Schiller, D., Alessandra, N. C., Alia-Klein, N., Becker, S., Cromwell, H. C., Dolcos, F., ... & Smith, R. C. (2022). The human affectome. https://doi.org/10.31234/osf.io/9nu32
Sturmberg, J. P., Picard, M., Aron, D. C., Bennett, J. M., Bircher, J., deHaven, M. J., Gijzel, S. M. W., Heng, H. H., Marcum, J. A., Martin, C. M., Miles, A., Peterson, C. L., Rohleder, N., Walker, C., Olde Rikkert, M. G. M., & Melis, R. J. F. (2019). Health and Disease-Emergent States Resulting From Adaptive Social and Biological Network Interactions. Frontiers in medicine, 6, 59. https://doi.org/10.3389/fmed.2019.00059
Rio, E., Kidgell, D., Moseley, G. L., Gaida, J., Docking, S., Purdam, C., & Cook, J. (2016). Tendon neuroplastic training: changing the way we think about tendon rehabilitation: a narrative review. British journal of sports medicine, 50(4), 209–215. https://doi.org/10.1136/bjsports-2015-095215
Wand, B. M., Cashin, A. G., McAuley, J. H., Bagg, M. K., Orange, G. M., & Moseley, G. L. (2022). The Fit-for-Purpose Model: Conceptualizing and Managing Chronic Nonspecific Low Back Pain as an Information Problem. Physical therapy, pzac151. Advance online publication. https://doi.org/10.1093/ptj/pzac151
Weng, H. Y., Feldman, J. L., Leggio, L., Napadow, V., Park, J., & Price, C. J. (2021). Interventions and Manipulations of Interoception. Trends in neurosciences, 44(1), 52–62. https://doi.org/10.1016/j.tins.2020.09.010
Zullo, A., Fleckenstein, J., Schleip, R., Hoppe, K., Wearing, S., & Klingler, W. (2020). Structural and Functional Changes in the Coupling of Fascial Tissue, Skeletal Muscle, and Nerves During Aging. Frontiers in physiology, 11, 592. https://doi.org/10.3389/fphys.2020.00592