Massage Therapy for People with Tendon Pain
/For people with tendon pain exercise therapy and load-management are first line treatment. In addition, manual therapy may be a useful adjunct to help manage pain and other associated symptoms (Irby et al., 2020; Jayaseelan et al., 2022).
Massage Therapy for People with Tendon Pain
Tendinopathy is the preferred term for persistent tendon pain and loss of function related to mechanical loading (Scott et al., 2020). In addition to a local tendon pathology a biopsychosocial approach to tendinopathy acknowledges and addresses the biological, psychological, and social contributions to pain and disability (Ackermann et al., 2022; Edger et al., 2022).
Patellar tendinopathy refers to persistent patellar tendon pain and loss of function related to mechanical loading.
Achilles tendinopathy refers to persistent Achilles tendon pain and loss of function related to mechanical loading.
Peroneal (fibularis) tendinopathy refers to persistent peroneal (fibularis) tendon pain and loss of function related to mechanical loading.
Medial or lateral elbow tendinopathy refers to persistent medial or lateral elbow tendon pain and loss of function related to mechanical loading.
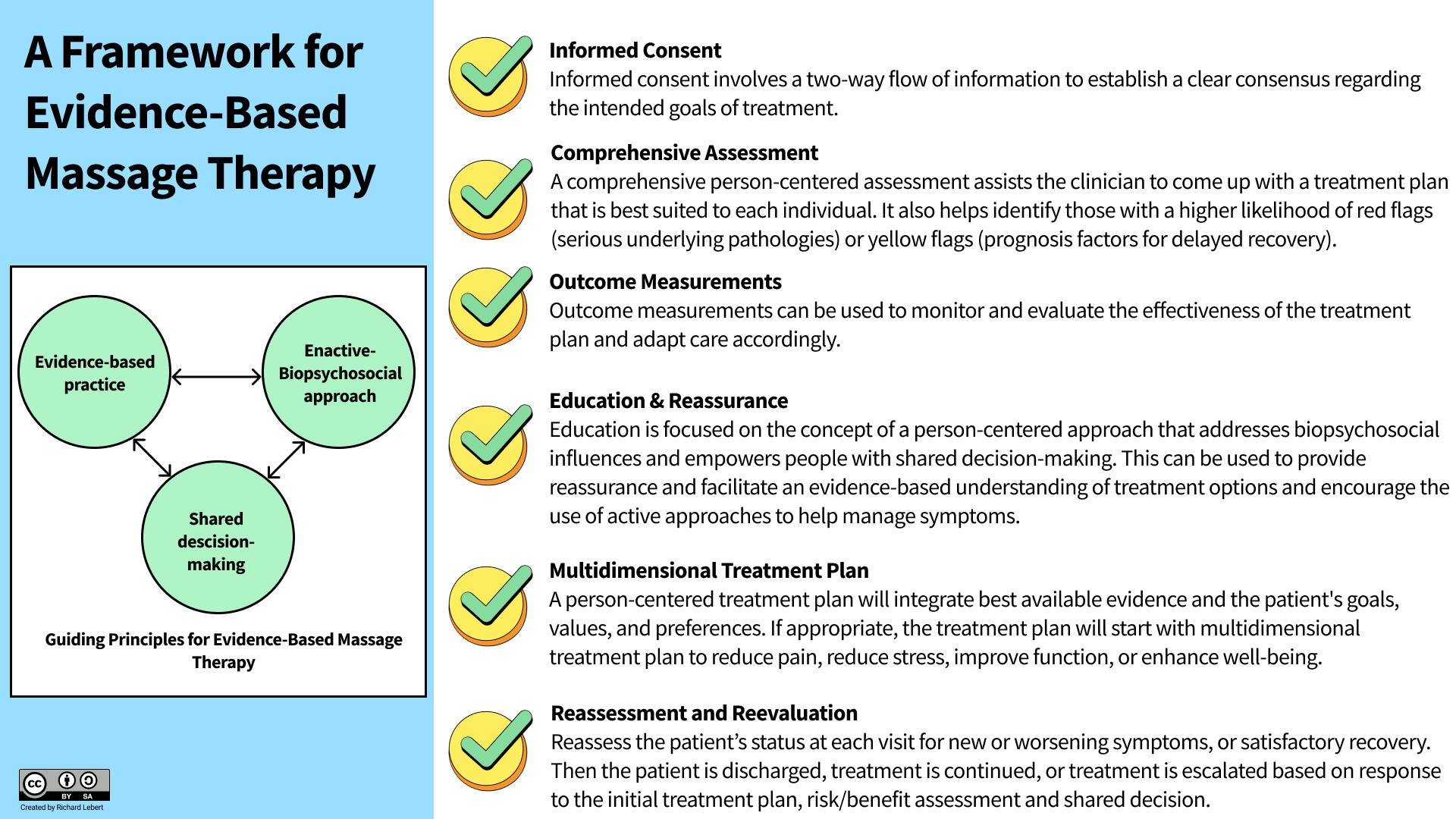
A Framework for Evidence-Based Massage Therapy
For people with tendon pain a multidisciplinary approach including exercise therapy and load-management are first line treatments. In addition, manual therapy may be a useful adjunct to help manage pain and other associated symptoms (Irby et al., 2020; Jayaseelan et al., 2022).
Here is a useful framework to help bridge the gap between research and the clinical application of massage therapy (informed by Caneiro et al., 2022; Cormack et al., 2022; Hoffmann et al., 2022; Hutting et al., 2022; Jesus et al., 2022; Kennedy et al., 2016; Kerns et al., 2022; Lin et al., 2020).
Informed Consent
Informed consent will include a discussion about natural history and the effects of no treatment, as well as the possible risks and benefits of receiving treatment. The therapist and patient will then work together to develop a plan of care based on the individualized goals and needs of the patient. This approach gives people the opportunity to be engaged in their own health through the process of shared decision making.
Comprehensive Assessment
A comprehensive assessment assists the clinician come up with a treatment plan that is best suited to each individual. It may involve a physical examination and detailed health history intake to gather information about patients' limitations, course of pain and can help identify those with a higher likelihood of red flags (serious underlying pathologies) or yellow flags (prognosis factors for delayed recovery). This may also help establish therapeutic alliance and identify the biological, psychological, social and contextual factors contributing to pain and disability.
Physical Examination - A physical examination could include palpation, observing gait, neurological screening tests, assessing mobility and/or muscle strength. Interpret examination results in the context of all assessment findings and implement an individualized treatment plan that is based on the assessment findings and goals of the patient.
Red Flags (serious underlying pathologies) - Red flags are signs and symptoms that raise suspicion of serious underlying pathology, if a serious pathology is suspected a clinical decision should be made to refer the patient to an appropriate healthcare practitioner. For the general population there are several red flags to be mindful of such as, substantial motor/sensory loss or progressive neurological deficits, fractures or osteoporosis risk/fragility fracture, acute infection, joint dislocation, and venous thromboembolism.
Yellow Flags (risk factors for delayed recovery) - This assessment process could also include screening questionnaires, such as the Orebro musculoskeletal pain questionnaire or Optimal Screening for Prediction of Referral and Outcome Yellow Flag (OSPRO-YF) to help identify yellow flags or identify patients at risk of poor prognosis. If the patient develops worsening physical or psychological symptoms consider a referral to counseling or an appropriate healthcare professional for further evaluation.
Outcome Measurements
Clinicians should use appropriate tools and strategies to monitor and evaluate the effectiveness of the treatment plan and adapt care accordingly. This could include incorporating one or more of the following outcome measurements when assessing and monitoring patient progress:
Self-Rated Recovery Question
Patient Specific Functional Scale
Brief Pain Inventory (BPI)
Visual Analog Scale (VAS)
Wearable Activity Tracker
Education & Reassurance
Focus on the concept of a person-centered approach that addresses biopsychosocial influences and empowers people with shared decision-making. Provide reassurance and facilitate an evidence based understanding of treatment options and encourage the use of active approaches (lifestyle, physical activity) to help manage symptoms. Reassess the patient’s status at each visit for new or worsening symptoms, or satisfactory recovery.
Multidimensional Treatment Plan
Manual Therapy - A massage therapy treatment plan should be implemented based on patient-specific assessment findings and patient tolerance. There may be times that focal irritability (i.e., nerve irritation, trigger points, nervous system sensitization) co-exists with tendon pain. Gently stretching the muscles, neurovascular structures, and investing fascia activates endogenous pain modulating systems that help to modulate neuro-immune responses.
Self-Management Strategies - Clinicians managing tendon pain should be thoughtful and skilled in managing the load on the tendons and supporting structures through a number of rehabilitation considerations. Self-management strategies such as isometric exercises, hydrotherapy, and relative rest may be useful for people with tendon pain.
Clinicians should work in partnership with patients to develop a person-centered care plan that considers best available evidence and the patient's goals, values, and preferences.
Reassessment and Reevaluation
Reassess the patient’s status at each visit for new or worsening symptoms, or satisfactory recovery. Then the patient is discharged, treatment is continued, or treatment is escalated based on response to the initial treatment plan, risk/benefit assessment and shared decision making.
References and Sources
Ackermann, P. W., Alim, M. A., Pejler, G., & Peterson, M. (2022). Tendon pain - what are the mechanisms behind it?. Scandinavian journal of pain, 10.1515/sjpain-2022-0018. Advance online publication. https://doi.org/10.1515/sjpain-2022-0018
Bayer, M. L., Magnusson, S. P., Kjaer, M., & Tendon Research Group Bispebjerg (2017). Early versus Delayed Rehabilitation after Acute Muscle Injury. The New England journal of medicine, 377(13), 1300–1301. doi:10.1056/NEJMc1708134
Bayer, M. L., Bang, L., Hoegberget-Kalisz, M., Svensson, R. B., Olesen, J. L., Karlsson, M. M., … Kjaer, M. (2019). Muscle-strain injury exudate favors acute tissue healing and prolonged connective tissue formation in humans. FASEB journal: official publication of the Federation of American Societies for Experimental Biology, 33(9), 10369–10382. doi:10.1096/fj.201900542R
Berrueta, L., Muskaj, I., Olenich, S., Butler, T., Badger, G. J., Colas, R. A., … Langevin, H. M. (2016). Stretching Impacts Inflammation Resolution in Connective Tissue. Journal of cellular physiology, 231(7), 1621–1627. doi:10.1002/jcp.25263
Best, T. M., Gharaibeh, B., & Huard, J. (2013). Stem cells, angiogenesis and muscle healing: a potential role in massage therapies?. British journal of sports medicine, 47(9), 556–560. doi:10.1136/bjsports-2012-091685
Bojsen-Møller, J., & Magnusson, S. P. (2019). Mechanical properties, physiological behavior, and function of aponeurosis and tendon. Journal of applied physiology (Bethesda, Md. : 1985), 126(6), 1800–1807. doi:10.1152/japplphysiol.00671.2018
Bove, G. M., Harris, M. Y., Zhao, H., & Barbe, M. F. (2016). Manual therapy as an effective treatment for fibrosis in a rat model of upper extremity overuse injury. Journal of the neurological sciences, 361, 168–180. doi:10.1016/j.jns.2015.12.029
Bove, G. M., Delany, S. P., Hobson, L., Cruz, G. E., Harris, M. Y., Amin, M., … Barbe, M. F. (2019). Manual therapy prevents onset of nociceptor activity, sensorimotor dysfunction, and neural fibrosis induced by a volitional repetitive task. Pain, 160(3), 632–644. doi:10.1097/j.pain.0000000000001443
Cardoso, T. B., Pizzari, T., Kinsella, R., Hope, D., & Cook, J. L. (2019). Current trends in tendinopathy management. Best practice & research. Clinical rheumatology, 33(1), 122–140. https://doi.org/10.1016/j.berh.2019.02.001
Challoumas, D., Clifford, C., Kirwan, P., & Millar, N. L. (2019). How does surgery compare to sham surgery or physiotherapy as a treatment for tendinopathy? A systematic review of randomised trials. BMJ open sport & exercise medicine, 5(1), e000528. https://doi.org/10.1136/bmjsem-2019-000528
Challoumas, D., Pedret, C., Biddle, M., Ng, N., Kirwan, P., Cooper, B., Nicholas, P., Wilson, S., Clifford, C., & Millar, N. L. (2021). Management of patellar tendinopathy: a systematic review and network meta-analysis of randomised studies. BMJ open sport & exercise medicine, 7(4), e001110. https://doi.org/10.1136/bmjsem-2021-001110
Clifford, C., Challoumas, D., Paul, L., Syme, G., & Millar, N. L. (2020). Effectiveness of isometric exercise in the management of tendinopathy: a systematic review and meta-analysis of randomised trials. BMJ open sport & exercise medicine, 6(1), e000760. https://doi.org/10.1136/bmjsem-2020-000760
Docking, S. I., & Cook, J. (2019). How do tendons adapt? Going beyond tissue responses to understand positive adaptation and pathology development: A narrative review. Journal of musculoskeletal & neuronal interactions, 19(3), 300–310.
Dubois, B., & Esculier, J. F. (2020). Soft-tissue injuries simply need PEACE and LOVE. British journal of sports medicine, 54(2), 72–73. https://doi.org/10.1136/bjsports-2019-101253
Duchesne, E., Dufresne, S. S., & Dumont, N. A. (2017). Impact of Inflammation and Anti-inflammatory Modalities on Skeletal Muscle Healing: From Fundamental Research to the Clinic. Physical therapy, 97(8), 807–817. doi:10.1093/ptj/pzx056
Dunn, S. L., & Olmedo, M. L. (2016). Mechanotransduction: Relevance to Physical Therapist Practice-Understanding Our Ability to Affect Genetic Expression Through Mechanical Forces. Physical therapy, 96(5), 712–721. doi:10.2522/ptj.20150073
Edgar, N., Clifford, C., O'Neill, S., Pedret, C., Kirwan, P., & Millar, N. L. (2022). Biopsychosocial approach to tendinopathy. BMJ open sport & exercise medicine, 8(3), e001326. https://doi.org/10.1136/bmjsem-2022-001326
Edwards, W. B. (2018). Modeling Overuse Injuries in Sport as a Mechanical Fatigue Phenomenon. Exercise and sport sciences reviews, 46(4), 224–231. doi:10.1249/JES.0000000000000163
Gracey, E., Burssens, A., Cambré, I., Schett, G., Lories, R., McInnes, I. B., Asahara, H., & Elewaut, D. (2020). Tendon and ligament mechanical loading in the pathogenesis of inflammatory arthritis. Nature reviews. Rheumatology, 16(4), 193–207. https://doi.org/10.1038/s41584-019-0364-x
Hamilton, B., Alonso, J. M., & Best, T. M. (2017). Time for a paradigm shift in the classification of muscle injuries. Journal of sport and health science, 6(3), 255–261. doi:10.1016/j.jshs.2017.04.011
Hunt, E. R., Baez, S. E., Olson, A. D., Butterfield, T. A., & Dupont-Versteegden, E. (2019). Using Massage to Combat Fear-Avoidance and the Pain Tension Cycle. International Journal of Athletic Therapy and Training, 24(5), 198-201.
Hunt, E. R., Confides, A. L., Abshire, S. M., Dupont-Versteegden, E. E., & Butterfield, T. A. (2019). Massage increases satellite cell number independent of the age-associated alterations in sarcolemma permeability. Physiological reports, 7(17), e14200. doi:10.14814/phy2.14200
Hsu, J. R., Mir, H., Wally, M. K., Seymour, R. B., & Orthopaedic Trauma Association Musculoskeletal Pain Task Force (2019). Clinical Practice Guidelines for Pain Management in Acute Musculoskeletal Injury. Journal of orthopaedic trauma, 33(5), e158–e182. doi:10.1097/BOT.0000000000001430
Irby, A., Gutierrez, J., Chamberlin, C., Thomas, S. J., & Rosen, A. B. (2020). Clinical management of tendinopathy: A systematic review of systematic reviews evaluating the effectiveness of tendinopathy treatments. Scandinavian journal of medicine & science in sports, 30(10), 1810–1826. https://doi.org/10.1111/sms.13734
Jayaseelan, D. J., Sault, J. D., & Fernandez-de-Las-Penas, C. (2022). Manual therapy should not be on the sideline in the game of treating tendinopathy. The Journal of manual & manipulative therapy, 1–6. Advance online publication. https://doi.org/10.1080/10669817.2022.2047269
Magnusson, S. P., & Kjaer, M. (2019). The impact of loading, unloading, ageing and injury on the human tendon. The Journal of physiology, 597(5), 1283–1298. doi:10.1113/JP275450
McGorm, H., Roberts, L. A., Coombes, J. S., & Peake, J. M. (2018). Turning Up the Heat: An Evaluation of the Evidence for Heating to Promote Exercise Recovery, Muscle Rehabilitation and Adaptation. Sports medicine (Auckland, N.Z.), 48(6), 1311–1328. doi:10.1007/s40279-018-0876-6
Millar, N. L., Murrell, G., & Kirwan, P. (2020). Time to put down the scalpel? The role of surgery in tendinopathy. British journal of sports medicine, 54(8), 441–442. https://doi.org/10.1136/bjsports-2019-101084
Millar, N. L., Silbernagel, K. G., Thorborg, K., Kirwan, P. D., Galatz, L. M., Abrams, G. D., Murrell, G., McInnes, I. B., & Rodeo, S. A. (2021). Tendinopathy. Nature reviews. Disease primers, 7(1), 1. https://doi.org/10.1038/s41572-020-00234-1
Miller, B. F., Hamilton, K. L., Majeed, Z. R., Abshire, S. M., Confides, A. L., Hayek, A. M., … Dupont-Versteegden, E. E. (2018). Enhanced skeletal muscle regrowth and remodelling in massaged and contralateral non-massaged hindlimb. The Journal of physiology, 596(1), 83–103. doi:10.1113/JP275089
Moseley, G. L., Baranoff, J., Rio, E., Stewart, M., Derman, W., & Hainline, B. (2018). Nonpharmacological Management of Persistent Pain in Elite Athletes: Rationale and Recommendations. Clinical journal of sport medicine: official journal of the Canadian Academy of Sport Medicine, 28(5), 472–479. doi:10.1097/JSM.0000000000000601
Rice, S. M., Gwyther, K., Santesteban-Echarri, O., Baron, D., Gorczynski, P., Gouttebarge, V., … Purcell, R. (2019). Determinants of anxiety in elite athletes: a systematic review and meta-analysis. British journal of sports medicine, 53(11), 722–730. doi:10.1136/bjsports-2019-100620
Rio, E., Moseley, L., Purdam, C., Samiric, T., Kidgell, D., Pearce, A. J., … Cook, J. (2014). The pain of tendinopathy: physiological or pathophysiological?. Sports medicine (Auckland, N.Z.), 44(1), 9–23. doi:10.1007/s40279-013-0096-z
Rio, E., & Docking, S. I. (2018). Adaptation of the pathological tendon: you cannot trade in for a new one, but perhaps you don't need to?. British journal of sports medicine, 52(10), 622–623. doi:10.1136/bjsports-2016-097325
Scott, A., Squier, K., Alfredson, H., Bahr, R., Cook, J. L., Coombes, B., … Zwerver, J. (2020). ICON 2019: International Scientific Tendinopathy Symposium Consensus: Clinical Terminology. British journal of sports medicine, 54(5), 260–262. https://doi.org/10.1136/bjsports-2019-100885
Stern, B. D., Hegedus, E. J., & Lai, Y. C. (2020). Injury prediction as a non-linear system. Physical therapy in sport: official journal of the Association of Chartered Physiotherapists in Sports Medicine, 41, 43–48. https://doi.org/10.1016/j.ptsp.2019.10.010
Thompson, W. R., Scott, A., Loghmani, M. T., Ward, S. R., & Warden, S. J. (2016). Understanding Mechanobiology: Physical Therapists as a Force in Mechanotherapy and Musculoskeletal Regenerative Rehabilitation. Physical therapy, 96(4), 560–569. doi:10.2522/ptj.20150224
van der Vlist, A. C., Winters, M., Weir, A., Ardern, C. L., Welton, N. J., Caldwell, D. M., Verhaar, J., & de Vos, R. J. (2021). Which treatment is most effective for patients with Achilles tendinopathy? A living systematic review with network meta-analysis of 29 randomised controlled trials. British journal of sports medicine, 55(5), 249–256. https://doi.org/10.1136/bjsports-2019-101872
Vicenzino, B., de Vos, R. J., Alfredson, H., Bahr, R., Cook, J. L., Coombes, B. K., … Zwerver, J. (2020). ICON 2019-International Scientific Tendinopathy Symposium Consensus: There are nine core health-related domains for tendinopathy (CORE DOMAINS): Delphi study of healthcare professionals and patients. British journal of sports medicine, 54(8), 444–451. https://doi.org/10.1136/bjsports-2019-100894