Neurodynamics (Research Notes)
/A recent meta-analysis published in The Journal of Orthopaedic & Sports Physical Therapy suggests that neurodynamic techniques may be useful for patients with back, neck and foot pain (Basson et al. 2017).
What is Neurodynamics?
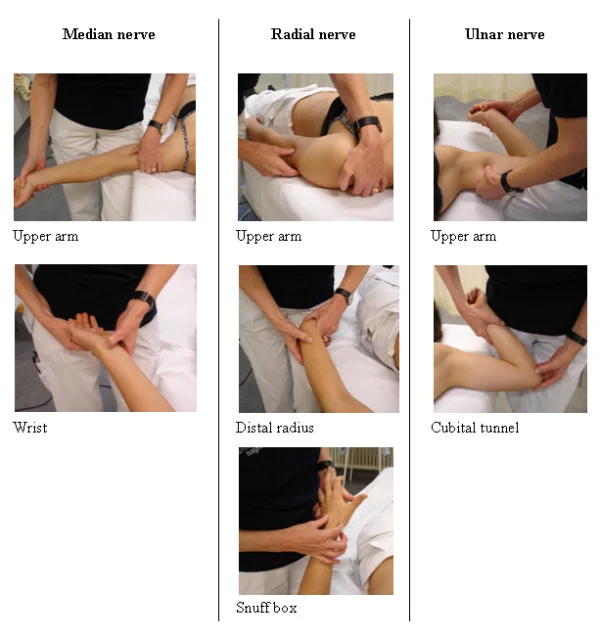
UPPER LIMB PERIPHERAL NERVE PALPATION POINTS (SCHMID ET AL. 2009).
Neurodynamics - “A clinical concept that uses movement (1) to assess increased mechanosensitivity of the nervous system; and (2) to restore the altered homeostasis in and around the nervous system.” (Grieve's Modern Musculoskeletal Physiotherapy).
Neurodynamic Assessment
Therapists often use neurodynamic movements to tension major nerves of the limbs to help identify sites of inflammation and/or irritation. Palpation of an involved nerve is another way to investigate symptoms (Schmid et al. 2009).
In cases of deep radiating pain, therapists may search for areas along the entire path of the involved nerve for tenderness.
Neurodynamic Treatments: A Biophyschosocial Framework
A biopsychosocial framework helps put into context the interconnected and multidirectional interaction between: physiology, thoughts, emotions, behaviors, culture, and beliefs. In terms of clinical responses to therapy there are a couple of proposed mechanisms of action, including but not limited to:
Pain Management
Neurodynamic movements have a modulatory affect on peripheral and central processes. This anti-nociceptive effect of massage therapy can help ease discomfort in patients who suffer from nerve irritation (Bishop et al. 2015, Vigotsky et al. 2015).
Sensitivities of Axons Exposed to a Pathological Environment
Neurovascular bundles may be exposed to mechanical irritation at many different points. Prolonged irritation may result in a reduction of intraneural blood flow. In turn, local hypoxia of a peripheral nerve leads to a drop in tissue pH that triggers the release of inflammatory mediators, known as “inflammatory soup”. This noxious substance can disrupt the normal function of nerves (Fisher et al. 2015). The application of specific soft tissue treatment may help to diminish intraneural edema and/or pressure by mobilizing neural tubes (Gilbert et al. 2015).
Inflammation and Mechanical Pressure are Interrelated
Ongoing tissue hypoxia or inflammatory responses lead to molecular signaling that promote the development of fibrosis, this may contribute to further peripheral nerve dysfunction (Fisher et al. 2015). The application of appropriate shear force and pressure impart a mechanical stimulus that may attenuate tissue levels of fibrosis and TGF-β1 (Bove et al. 2016).
Key Point
Non-pharmacological therapeutic interventions are being embraced by the medical community because they are often simple to carry out, economical, and have relatively minor side effects (Busse et al. 2017, Chou et al. 2017, Nahin et al. 2016, Qaseem et al. 2017).
Nerve mobilizations are non-pharmacological options for musculoskeletal pain that patients can discuss with their physician. None of these options are a panacea, but they may help you put together a individualized multi-modal program to manage persistent symptoms
More to Explore
Related Links
• Massage Therapy Research
• Biopsychosocial Model of Massage Therapy
• Myofascial Techniques
• Sports Massage
• Active Release Treatments
• Medical Acupuncture
• Cupping
• Taping
• IASTM
Research Links
Baselgia, L.T., Bennett, D.L., Silbiger, R.M., Schmid, A.B. (2017). Negative Neurodynamic Tests Do Not Exclude Neural Dysfunction in Patients With Entrapment Neuropathies. Arch Phys Med Rehabil.
https://www.ncbi.nlm.nih.gov/pubmed/27449322
Basson, A., Olivier, B., Ellis, R., Coppieters, M., Stewart, A., Mudzi, W. (2017). The Effectiveness of Neural Mobilization for Neuro-Musculoskeletal Conditions: A Systematic Review and Meta-Analysis. J Orthop Sports Phys Ther.
https://www.ncbi.nlm.nih.gov/pubmed/28704626
Berrueta, L., Muskaj, I., Olenich, S., Butler, T., Badger, G. J., Colas, R. A., . . . Langevin, H. M. (2016). Stretching Impacts Inflammation Resolution in Connective Tissue. Journal of Cellular Physiology.
http://www.ncbi.nlm.nih.gov/pubmed/26588184
Bishop, M. D., Torres-Cueco, R., Gay, C. W., Lluch-Girbés, E., Beneciuk, J. M., & Bialosky, J. E. (2015). What effect can manual therapy have on a patient's pain experience? Pain Management.
https://www.ncbi.nlm.nih.gov/pubmed/26401979
Boudier-Revéret, M., Gilbert, K.K., Sobczak, S. (2017). Effect of neurodynamic mobilization on fluid dispersion in median nerve at the level of the carpal tunnel: A cadaveric study. Musculoskelet Sci Pract.
https://www.ncbi.nlm.nih.gov/pubmed/28734168
Bove, G.M., Harris, M.Y., Zhao, H., Barbe, M.F. (2016). Manual therapy as an effective treatment for fibrosis in a rat model of upper extremity overuse injury. J Neurol Sci.
https://www.ncbi.nlm.nih.gov/pubmed/26810536
Bove, G.M. (2008). Epi-perineurial anatomy, innervation, and axonal nociceptive mechanisms. J Bodyw Mov Ther.
https://www.ncbi.nlm.nih.gov/pubmed/19083672
Chang, K.V., Lin, C.P., ... Özçakar, L. (2017). Sonographic tracking of trunk nerves: essential for ultrasound-guided pain management and research. J Pain Res.
https://www.ncbi.nlm.nih.gov/pubmed/28115867
Chen, L., Michalsen, A. (2017). Management of chronic pain using complementary and integrative medicine. BMJ.
https://www.ncbi.nlm.nih.gov/pubmed/28438745
Coppieters, M.W., Butler, D.S. (2008). Do 'sliders' slide and 'tensioners' tension? An analysis of neurodynamic techniques and considerations regarding their application. Man Ther.
https://www.ncbi.nlm.nih.gov/pubmed/17398140/
Dilley, A., Lynn, B., Pang, S.J. (2005). Pressure and stretch mechanosensitivity of peripheral nerve fibres following local inflammation of the nerve trunk. Pain.
https://www.ncbi.nlm.nih.gov/pubmed/16154692
Dong, Q., Jacobson, J.A., ... Kim, S.M. (2012). Entrapment neuropathies in the upper and lower limbs: anatomy and MRI features. Radiol Res Pract.
https://www.ncbi.nlm.nih.gov/pubmed/23125929
Fisher, P., Zhao, Y., Rico, M., Massicotte, V., Wade, C., Litvin, J., . . . Barbe, M. (2015). Increased CCN2, substance P and tissue fibrosis are associated with sensorimotor declines in a rat model of repetitive overuse injury. Journal of Cell Communication and Signaling.
https://www.ncbi.nlm.nih.gov/pubmed/25617052 (OPEN ACCESS)
Gao, F., Xiang, H.C., ... Li, M. (2017). Electroacupuncture Inhibits NLRP3 Inflammasome Activation through CB2 Receptors in Inflammatory Pain. Brain Behav Immun.
https://www.ncbi.nlm.nih.gov/pubmed/28782714
Gilbert, K. K., James, C. R., Apte, G., Brown, C., Sizer, P. S., Brismée, J., & Smith, M. P. (2015). Effects of simulated neural mobilization on fluid movement in cadaveric peripheral nerve sections: Implications for the treatment of neuropathic pain and dysfunction. Journal of Manual & Manipulative Therapy. (OPEN ACCESS)
http://www.ncbi.nlm.nih.gov/pubmed/26917940
Gilbert, K.K., Smith, M.P., Sobczak, S.,.... Brismée, J.M. (2015). Effects of lower limb neurodynamic mobilization on intraneural fluid dispersion of the fourth lumbar nerve root: an unembalmed cadaveric investigation. J Man Manip Ther. (OPEN ACCESS)
https://www.ncbi.nlm.nih.gov/pubmed/26955255
Govea, R.M., Barbe, M.F., Bove, G.M. (2017). Group IV nociceptors develop axonal chemical sensitivity during neuritis and following treatment of the sciatic nerve with vinblastine. J Neurophysiol.
https://www.ncbi.nlm.nih.gov/pubmed/28701542
Iyengar, S., Ossipov, M.H., Johnson, K.W. (2017). The role of calcitonin gene-related peptide in peripheral and central pain mechanisms including migraine. Pain.
https://www.ncbi.nlm.nih.gov/pubmed/28301400
Jeong, U.C., Kim, C.Y., Park, Y.H., Hwang-Bo, G., Nam, C.W. (2016). The effects of self-mobilization techniques for the sciatic nerves on physical functions and health of low back pain patients with lower limb radiating pain. J Phys Ther Sci.
https://www.ncbi.nlm.nih.gov/pubmed/26957726
Lee, H, et al., (2017). Causal mechanisms in the clinical course and treatment of back pain. Best Practice & Research Clinical Rheumatology.
http://www.sciencedirect.com/science/article/pii/S1521694217300013
Manvell, J.J., Manvell, N., Snodgrass, S.J., Reid, S.A. (2015). Improving the radial nerve neurodynamic test: An observation of tension of the radial, median and ulnar nerves during upper limb positioning. Man Ther.
https://www.ncbi.nlm.nih.gov/pubmed/25892706
Manvell, N., Manvell, J.J., Snodgrass, S.J., Reid, S.A. (2015). Tension of the ulnar, median, and radial nerves during ulnar nerve neurodynamic testing: observational cadaveric study. Phys Ther.
https://www.ncbi.nlm.nih.gov/pubmed/25592186
Nee, R.J., Jull, G.A., Vicenzino, B., Coppieters, M.W. (2012). The validity of upper-limb neurodynamic tests for detecting peripheral neuropathic pain. J Orthop Sports Phys Ther.
https://www.ncbi.nlm.nih.gov/pubmed/22402638
Neto, T., Freitas, S.R., Marques, M., Gomes, L., Andrade, R., Oliveira, R. (2017). Effects of lower body quadrant neural mobilization in healthy and low back pain populations: A systematic review and meta-analysis. Musculoskelet Sci Pract.
https://www.ncbi.nlm.nih.gov/pubmed/28637597
Olivo, R., Tsao, B. (2017). Peripheral Nerve Injuries in Sport. Neurol Clin.
https://www.ncbi.nlm.nih.gov/pubmed/28673416/
Quintner, J., Bove, G., & Cohen, M. (2015). A critical evaluation of the trigger point phenomenon. Rheumatology.
https://www.ncbi.nlm.nih.gov/pubmed/25477053
Rade, M., Pesonen, J., Airaksinen, O. (2017). Reduced Spinal Cord Movement With the Straight Leg Raise Test in Patients With Lumbar Intervertebral Disc Herniation. Spine (Phila Pa 1976).
https://www.ncbi.nlm.nih.gov/pubmed/28542104
Rodríguez-Sanz, D., López-López, D., ... Calvo-Lobo, C. (2017). Effects of Median Nerve Neural Mobilization in Treating Cervicobrachial Pain: A Randomized Waiting List-controlled Clinical Trial. Pain Pract.
https://www.ncbi.nlm.nih.gov/pubmed/28734105/
Schmid, A.B., Nee, R.J., Coppieters, M.W. (2013). Reappraising entrapment neuropathies--mechanisms, diagnosis and management. Man Ther.
https://www.ncbi.nlm.nih.gov/pubmed/24008054
Schmid, A. B., Brunner, F., ... Coppieters, M. W. (2009). Reliability of clinical tests to evaluate nerve function and mechanosensitivity of the upper limb peripheral nervous system. BMC Musculoskeletal Disorders.
https://www.ncbi.nlm.nih.gov/pubmed/19154625
Sluka, K.A., Clauw, D.J. (2016). Neurobiology of fibromyalgia and chronic widespread pain. Neuroscience.
https://www.ncbi.nlm.nih.gov/pubmed/27291641
Torres, J.R., Martos, I.C., ... Valenza, M.C. (2015). Results of an Active Neurodynamic Mobilization Program in Patients With Fibromyalgia Syndrome: A Randomized Controlled Trial. Arch Phys Med Rehabil.
https://www.ncbi.nlm.nih.gov/pubmed/26143052/
Urban, L.M., MacNeil, B.J. (2015). Diagnostic Accuracy of the Slump Test for Identifying Neuropathic Pain in the Lower Limb. J Orthop Sports Phys Ther.
https://www.ncbi.nlm.nih.gov/pubmed/26107044
Vigotsky, A. D., & Bruhns, R. P. (2015). The Role of Descending Modulation in Manual Therapy and Its Analgesic Implications: A Narrative Review. Pain Research and Treatment.
https://www.ncbi.nlm.nih.gov/pubmed/26788367 (OPEN ACCESS)