Whole-Person Health: An Integrated Approach to Musculoskeletal Health
/A Whole Person Approach is Shift away from the primarily tissue focused approach to one that looks at the health of the whole system.
Whole-Person Health: An Integrated Approach to Musculoskeletal Health
Moving Beyond Reductionism: A Whole-Person View
For thousands of years, people around the globe have utilized massage to address a wide range of health issues. Early healing traditions were often rooted in an ecological understanding of health and well-being. These traditions viewed the body as an ecosystem in delicate balance with its surroundings, constantly interacting with the environment and influenced by the natural world.
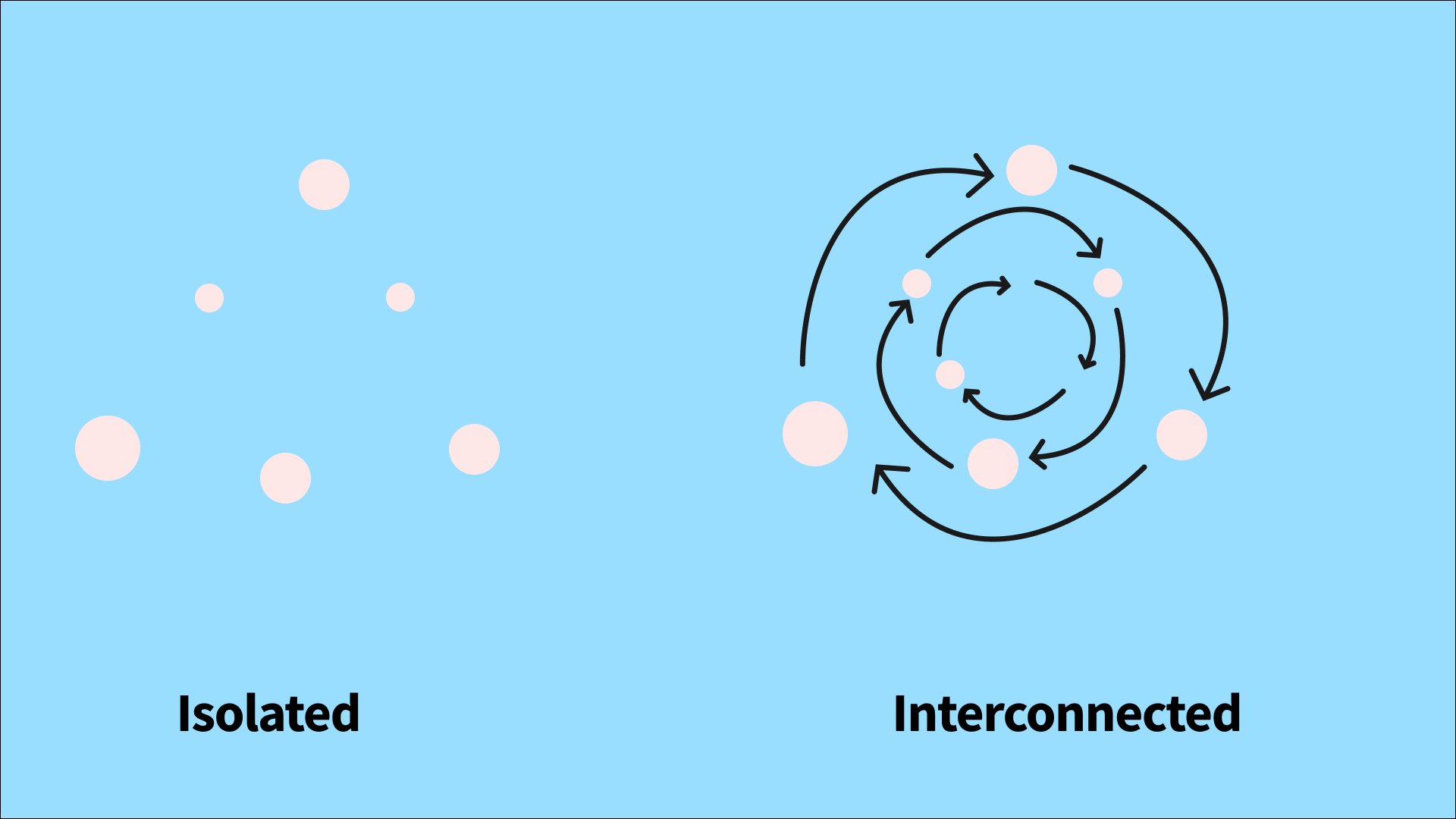
In musculoskeletal health today, modern medicine often defaults to reductionist, disease-centric models. These models often treat conditions in isolation, frequently overlooking the complex interplay of biological, psychological, social, and environmental factors. A paradigm shift toward Whole-Person Health necessitates a more holistic approach, deeply rooted in the principles of complexity science.
Complexity Science: A Lens for Musculoskeletal Health
Complexity science studies systems with numerous interconnected parts. It provides a useful framework for understanding musculoskeletal health by highlighting the non-linear relationships and interconnectedness of factors that influence health outcomes.
When we treat people with persistent musculoskeletal conditions—such as low back pain or osteoarthritis—we often realize that a "quick fix" fails because the condition is maintained by a complex interplay of factors. By "zooming out," we can ask the right questions:
What are the underlying interconnected issues?
Are there leverage points where a minor change can produce significant, disproportionate changes across the whole system?
Health, Well-Being, and Complex Systems
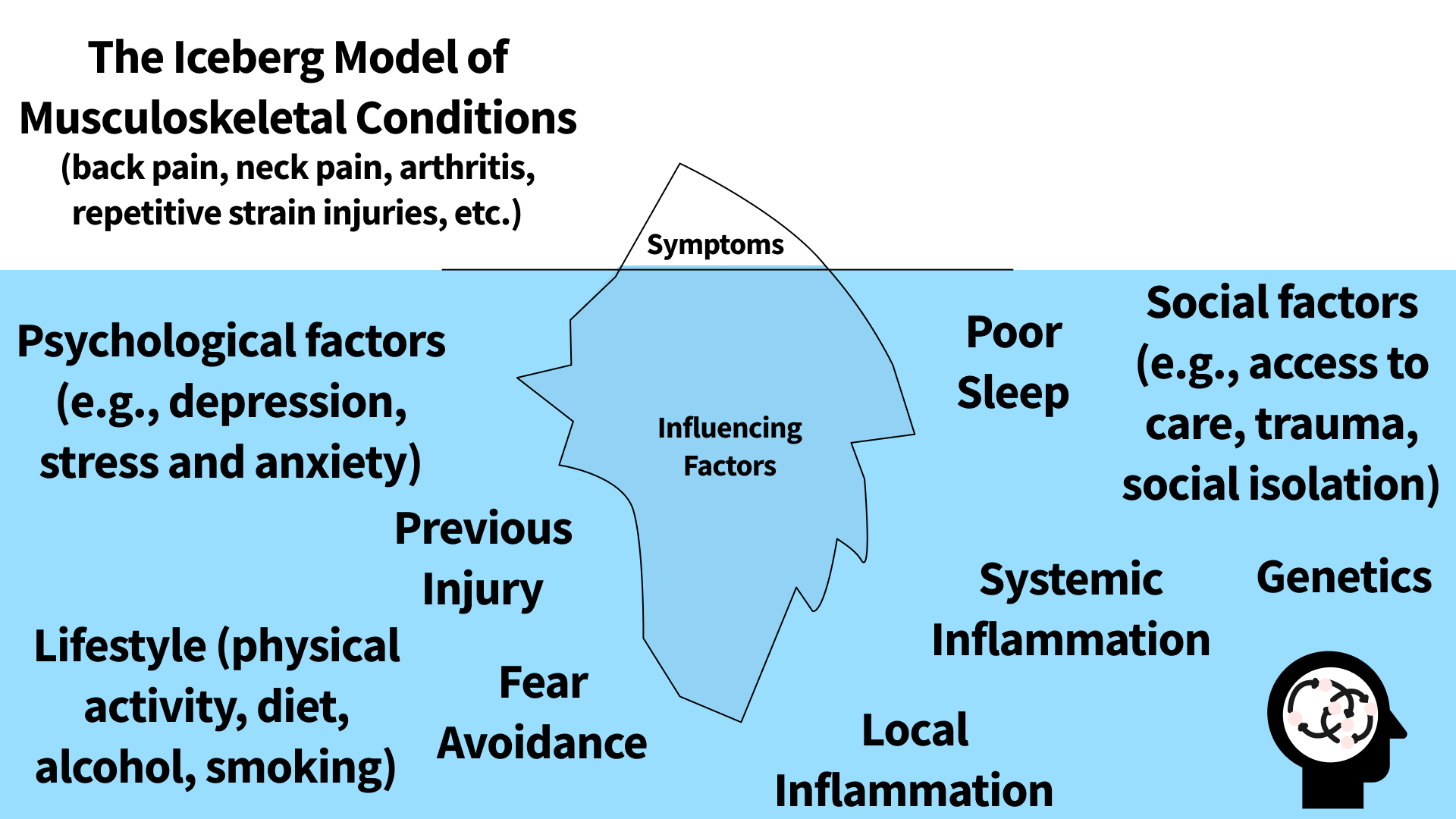
"Musculoskeletal conditions" is a broad term for problems affecting muscles, bones, joints, tendons, ligaments, and nerves (e.g., back pain, neck pain, arthritis, repetitive strain injuries). These conditions can be conceptualized as complex networks of interacting symptoms, such as pain, stiffness, poor sleep, and decreased activity.
Symptoms as Interconnected Nodes
Imagine each symptom as a "node" in a network. These nodes are not isolated; they are interconnected. For example, chronic pain can lead to poor sleep, which in turn reduces physical activity. Reduced activity can cause muscle weakness and greater stiffness, further worsening the pain.
Pharmacological and non-pharmacological treatments alter network dynamics, thereby disrupting the self-reinforcing cycle of interconnected symptoms.
The effects of an intervention cannot be explained by a single mechanism. Instead, it acts through a complex interplay of interconnected responses. This aligns with the concept of a "whole-person approach," which emphasizes the interconnectedness of biological, psychological, and social factors that contribute to our overall health and well-being.
Allostatic Load and Resilience
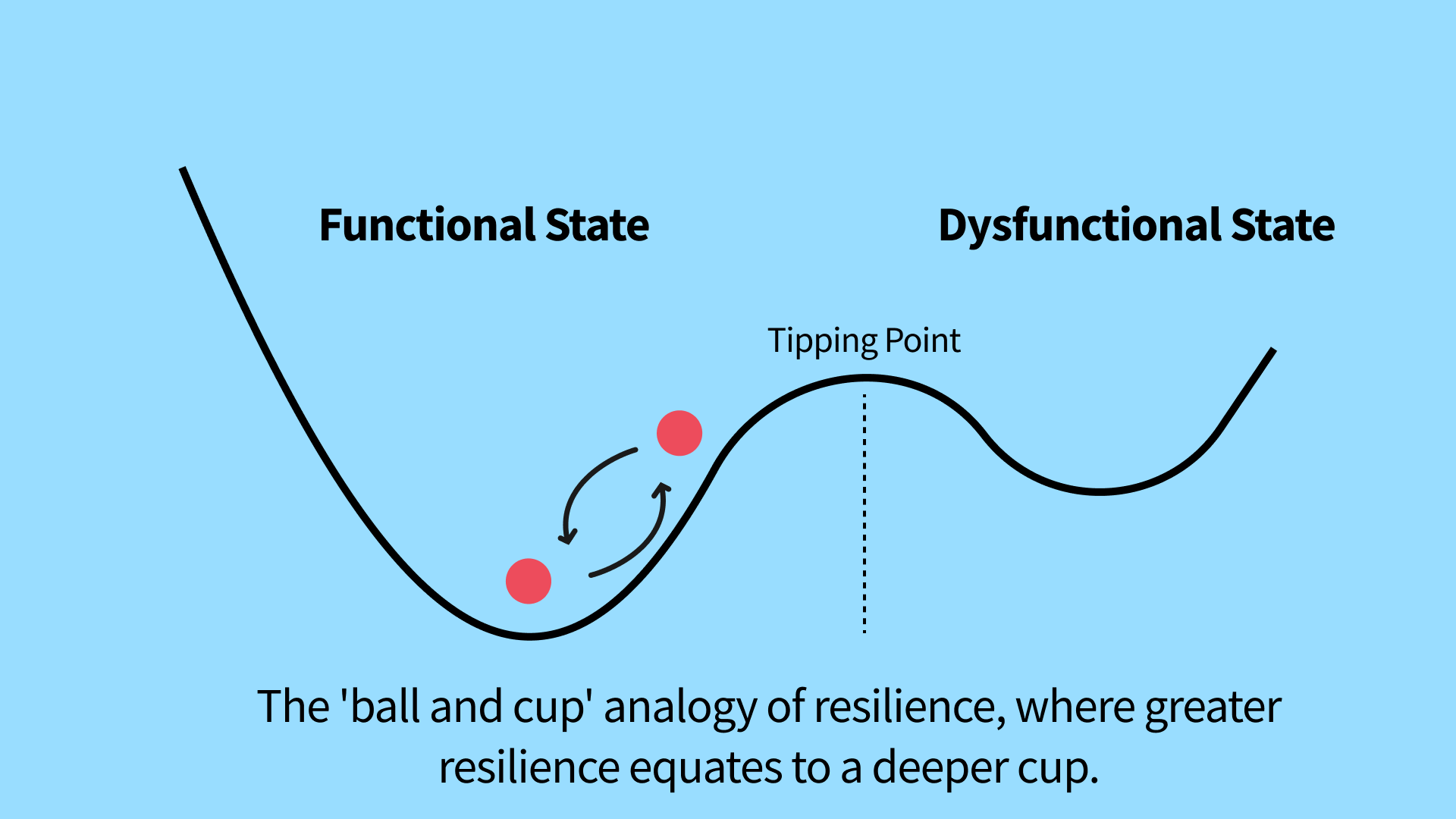
Health and well-being are emergent properties of these interactions, not just the sum of individual symptoms (Cohen et al., 2025). The body's capacity to maintain stability when facing chronic stressors is known as resilience. The "ball and cup" analogy is often used to illustrate this:
A deeper cup represents greater resilience, making the system less likely to be pushed past a tipping point into a dysfunctional, chronic state.
External and internal factors (e.g., trauma, systemic inflammation, poor sleep, depression, stress, anxiety) act as perturbations that nudge the system toward its tipping point (Lutke Schipholt et al., 2025).
The Whole-Person Health framework emphasizes an adaptability-focused approach to therapy (Pitcher et al., 2023). When an individual faces chronic stressors, the cumulative wear-and-tear is known as allostatic load. This load diminishes the body's natural resilience, contributing to the emergence and maintenance of chronic pain and musculoskeletal conditions. A key contributor to this is dysregulated neural-endocrine-immune responses (Chapman et al., 2008).
Key Idea: This approach views the system as a whole—where the whole is greater than the sum of its isolated parts—by recognizing how biological, psychological, social, and environmental factors are intertwined.
The 'ball and cup' analogy provides one of the clearest visuals to help understand how complex systems maintain stability and how they transition into new states. A complex system's stability is linked to the depth of the basin. Building resilience (the dashed line) in a system makes it less likely to be pushed past a tipping point into a dysfunctional state. Perturbations that may push the system towards its tipping point include trauma, systemic inflammation, physical inactivity, poor sleep, and psychological factors (such as depression, stress and anxiety symptoms).
Fostering Adaptability and Resilience
A complex systems approach informs the development of multidisciplinary strategies that aim to shift individuals toward a more resilient state. These treatments alter network dynamics through interconnected physiological, psychological, and social processes. Strategies that support lifestyle factors—such as sleep, stress management, nutrition, and physical activity—can have a profound effect on overall health (Artz et al., 2024; Deenik et al., 2025; Langevin et al., 2024; Nijs et al., 2024).
Multimodal Strategies to Foster Adaptability and Resilience:
Mind-Body Interventions: Reducing threat perception and improving emotional regulation (Quinlan et al., 2024; Wayne et al., 2025).
Physical Activity, Exercise and Movement: Increasing physiological capacity and promoting active coping (Dibben et al., 2024; Schütze et al., 2025).
Massage and Manual Therapy: Modulating the nervous system and reducing acute allostatic load (Jinich-Diamant et al., 2025; Keter et al., 2025; Packheiser et al., 2024; Shepherd et al., 2025).
Implications for Clinical Practice
Adopting this whole-person approach informs the development of context-specific multidisciplinary strategies that foster adaptability and resilience.
Benefits of a Whole-Person Health Approach:
Shift in View: Moving from a reductionist, isolated-symptom view to a dynamic, systems-level understanding of health and well-being.
Individualized Care: Tailoring treatment plans to address the specific, unique network of symptoms impacting each individual.
Improved Outcomes: Leading to more effective and sustainable improvements in function and well-being.
Key Message
The shift to Whole-Person Health necessitates an ecological understanding of well-being, one that views health as an intricate web of connected systems—not just within the individual body, but also in relation to their environment and social context. Embracing complexity science provides the foundation for comprehensive, evidence-based care.
“A shift toward Whole-Person Health recognizes that well-being isn’t just what’s happening in the body—it’s shaped by our environment, social context, and lived experiences.”
By shifting from a reductionist view to a systems-level view, we can foster adaptability and resilience through dynamic physiological, psychological, and social processes.
Glossary of Terms
Active inference: A normative framework that elucidates the neural and cognitive processes underlying sentient behavior, beginning with first principles. This framework posits that perception and action work in concert to minimize a shared functional known as variational free energy.
Allostasis: The flexible regulation of physiology, underwriting the maintenance of variables within specified ranges by pre-emptive responses based on current and predicted future physiological states, external environments, and behavioral goals.
Allostatic load: The “wear and tear” on the body associated with chronically high levels of stress and arousal.
Complex system: A system in which the properties are highly dependent on the interactions of its many parts, possibly involving feedback, cycles, and nonlinearities. In this context, “complex” should not be equated with “complicated.”
Critical transition: The point at which a system suddenly jumps from one equilibrium to another.
Enactivism: A perspective that emphasizes the active role of an organism in constructing and experiencing the world through its interactions with its environment.
Equilibrium: A state of a complex system in which current functioning tends to be maintained despite perturbations occurring over time.
Exteroception: Perceptual inference based on sensory signals originating from outside the body (e.g., vision, hearing, touch, taste, smell).
Force-based manipulations: The application of mechanical forces to the outside of the body with therapeutic intent. This can include light touch, soft tissue massage, mobilization, cupping, acupuncture, or other needling interventions.
Health: A state of physical, mental, and social well-being and not merely the absence of disease and infirmity.
Interoception: The processing of sensing and perceiving sensory signals relating to internal bodily states.
Musculoskeletal conditions: A broad term for problems that affect muscles, bones, joints, tendons, ligaments, and nerves.
Network dynamics: Changes of state in biological networks over time or the propagation of effects due to stimuli or disruptions; crucial for understanding disease progression and the impact of therapeutic interventions.
Neuroplasticity: Changes in neural pathways and synapses that result from bodily injury or changes in behavior, environment, or neural processes. This reflects the concept that the brain is a dynamic organ that constantly changes in response to internal and external events.
Non-linearity: A relationship where outputs are not always proportional to inputs. Small changes may lead to large changes in the system and vice versa.
Perturbation: An external factor that potentially interferes with the system’s behavior.
Resilience: A system's capacity to recover, grow, adapt, or resist perturbation from a challenge or stressor.
Salutogenesis: The process by which individuals move from a less healthy state to a healthier state. The concept emphasizes factors that promote and maintain good health rather than focusing solely on pathogenesis (disease).
Whole-person health: Involves examining interconnections among all organs and systems of the body, as well as the effects of multicomponent interventions across physiological, behavioral, social, and environmental domains.
References and Sources
With over 15 years of clinical experience and extensive study of massage therapy research, I'm committed to creating resources that foster the professional development of massage therapists globally. Whether you're a seasoned massage therapist or a curious newcomer, this massage therapy glossary is here to be your one-stop shop for understanding terms as it relates to massage therapy. Additionally this post highlights a substantial body of evidence supporting the use of massage therapy in alleviating pain and enhancing quality of life across a range of health issues.
This is a selection of sources I used to help formulate my ideas based on over-lapping concepts from massage therapy, physiotherapy, chiropractic, osteopathy, lifestyle medicine and traditional healing approaches.
Anjum, R. L., Copeland, S., Rocca E. (2020) Rethinking Causality, Complexity and Evidence for the Unique Patient. Springer Nature.
Ang, L., Song, E., Jong, M. C., Alræk, T., Wider, B., Choi, T. Y., Jun, J. H., Lee, B., Choi, Y., Lee, H. W., Yang, C., Yim, M. H., Yamashita, H., Ji, Z., Hu, H., Zhang, J., Liu, J., Chen, Y., Qin, Y., Lu, L., … Lee, M. S. (2024). An evidence map on traditional medicine across health outcomes. Integrative medicine research, 13(3), 101070. https://doi.org/10.1016/j.imr.2024.101070
Artz, K. E., Phillips, T. D., Moore, J. M., & Tibbe, K. E. (2024). Redesigning the Care of Musculoskeletal Conditions With Lifestyle Medicine. Mayo Clinic proceedings. Innovations, quality & outcomes, 8(5), 418–430. https://doi.org/10.1016/j.mayocpiqo.2024.07.001
Barbe, M. F., Lambi, A. G., Harris, M. Y., Patel, P. R., Tamas, I. P., McGonagle, E. R., Van Der Bas, M., Kalicharan, B. A., Bright-Rowe, L., Popoff, S. N., & Klyne, D. M. (2025). Overuse injury induces persistent behavioral declines that correlate with higher IL-6 expression in the affected musculoskeletal tissues, circulation, and brain. Frontiers in physiology, 16, 1500795. https://doi.org/10.3389/fphys.2025.1500795
Beinfield, H., & Korngold, E. (1995). Chinese traditional medicine: an introductory overview. Alternative therapies in health and medicine, 1(1), 44–52.
Borsook, D. (2025). Allostatic load and pain: instability of a bio-social ecosystem. Pain, 166(11S), S27–S32. https://doi.org/10.1097/j.pain.0000000000003716
Branchi l, I. (2025). Integrating plasticity into precision psychiatry. European psychiatry : the journal of the Association of European Psychiatrists, 68(1), e54. https://doi.org/10.1192/j.eurpsy.2025.19
Bringmann, L. F., Helmich, M. A., Eronen, M. I., & Voelkle, M. C. (2023). Complex systems approaches to psychopathology. In R. F. Krueger & P. H. Blaney (Eds.) Oxford Textbook of Psychopathology (4th ed., pp. 103-122). Oxford University Press. https://doi.org/10.1093/med-psych/9780197542521.003.0005
Buenrostro-Jáuregui, M. H., Muñóz-Sánchez, S., Rojas-Hernández, J., Alonso-Orozco, A. I., Vega-Flores, G., Tapia-de-Jesús, A., & Leal-Galicia, P. (2025). A Comprehensive Overview of Stress, Resilience, and Neuroplasticity Mechanisms. International journal of molecular sciences, 26(7), 3028. https://doi.org/10.3390/ijms26073028
Cashin, A. G., McAuley, J. H., Lamb, S. E., & Lee, H. (2021). Disentangling contextual effects from musculoskeletal treatments. Osteoarthritis and cartilage, 29(3), 297–299. https://doi.org/10.1016/j.joca.2020.12.011
Cerritelli, F., & Esteves, J. E. (2022). An Enactive-Ecological Model to Guide Patient-Centered Osteopathic Care. Healthcare (Basel, Switzerland), 10(6), 1092. https://doi.org/10.3390/healthcare10061092
Chapman, C. R., Tuckett, R. P., & Song, C. W. (2008). Pain and stress in a systems perspective: reciprocal neural, endocrine, and immune interactions. The journal of pain, 9(2), 122–145. https://doi.org/10.1016/j.jpain.2007.09.006
Cholewicki, J., Hodges, P. W., Popovich, J. M., Aminpour, P., Gray, S. A., Lee, A. S., Breen, A., Brumagne, S., van Dieën, J. H., Dillen, L. R. V., Dreisinger, T. E., Ferreira, M. L., George, S. Z., Goertz, C. M., Hartvigsen, J., Hides, J. A., Hoy, D., Kawchuk, G. N., Koes, B. W., Kothe, R., … Weiser, S. (2025). A meta-model of low back pain to examine collective expert knowledge of the effects of treatments and their mechanisms. Research square, rs.3.rs-7844247. https://doi.org/10.21203/rs.3.rs-7844247/v1
Cohen, A. A., Picard, M., Beard, J. R., Belsky, D. W., Herbstman, J., Kuryla, C. L., Liu, M., Makarem, N., Malinsky, D., Pei, S., Wei, Y., & Fried, L. P. (2025). Intrinsic health as a foundation for a science of health. Science advances, 11(25), eadu8437. https://doi.org/10.1126/sciadv.adu8437
Cook, C. E., Abraira, V. E., Burns, J., Degenhardt, B. F., Kawchuk, G., Keter, D., Loghmani, M. T., Reed, W. R., Winkelstein, B. A., & McDevitt, A. (2025). Categorizing Treatment Mechanisms for Complementary and Integrative Musculoskeletal Interventions. International journal of osteopathic medicine : IJOM, 55, 100749. https://doi.org/10.1016/j.ijosm.2025.100749
Cormack, B., Stilwell, P., Coninx, S., & Gibson, J. (2023). The biopsychosocial model is lost in translation: from misrepresentation to an enactive modernization. Physiotherapy theory and practice, 39(11), 2273–2288. https://doi.org/10.1080/09593985.2022.2080130
Coninx, S., & Stilwell, P. (2023). Chronic Pain, Enactivism, & the Challenges of Integration. In Situated Cognition Research: Methodological Foundations (pp. 241-276). Springer International Publishing.
d'Andrea, V., Loscalzo, J., & De Domenico, M. (2025). Challenges and opportunities in the network medicine of complex diseases. Med (New York, N.Y.), 100920. Advance online publication. https://doi.org/10.1016/j.medj.2025.100920
Deenik, J., Vermeulen, J. M., Teasdale, S. B., Schuch, F. B., Marx, W., Perry, B., Diez, G. G., Castellanos, N., Elshazly, M., Gatera, G., Waugh, M., Hepsomali, P., Bueno-Antequera, J., Borrueco Sánchez, J., Lopez Moral, A., López-Sánchez, C., Oviedo Caro, M. A., Dejonge, M., Noortman, C., van Schothorst, M., … Firth, J. (2025). Lifestyle psychiatry: a conceptual framework for application in mental healthcare and support. BMJ mental health, 28(1), e301980. https://doi.org/10.1136/bmjment-2025-301980
Dibben, G. O., Gardiner, L., Young, H. M. L., Wells, V., Evans, R. A., Ahmed, Z., Barber, S., Dean, S., Doherty, P., Gardiner, N., Greaves, C., Ibbotson, T., Jani, B. D., Jolly, K., Mair, F. S., McIntosh, E., Ormandy, P., Simpson, S. A., Ahmed, S., Krauth, S. J., … PERFORM research team (2024). Evidence for exercise-based interventions across 45 different long-term conditions: an overview of systematic reviews. EClinicalMedicine, 72, 102599. https://doi.org/10.1016/j.eclinm.2024.102599
Dunn, M., Rushton, A. B., Mistry, J., Soundy, A., & Heneghan, N. R. (2024). The biopsychosocial factors associated with development of chronic musculoskeletal pain. An umbrella review and meta-analysis of observational systematic reviews. PloS one, 19(4), e0294830. https://doi.org/10.1371/journal.pone.0294830
Friedman, Y. (2022). Who is the biological patient? A new gradational and dynamic model for one health medicine. History and philosophy of the life sciences, 44(4), 61. https://doi.org/10.1007/s40656-022-00540-9
Graham, K. D., Foley, H., Adams, J., & Steel, A. (2023). Complex systems, complex practice, complex outcomes: a call for the development of complexity-informed implementation models (CIIM) for traditional, complementary, and integrative medicine. European journal of integrative medicine, 64, 102314. https://doi.org/10.1016/j.eujim.2023.102314
Hardcastle, V. G. (2024). Entangled brains and the experience of pains. Frontiers in psychology, 15, 1359687. https://doi.org/10.3389/fpsyg.2024.1359687
Harrison, L. A., Gracias, A. J., Friston, K. J., & Buckwalter, J. G. (2025). Resilience phenotypes derived from an active inference account of allostasis. Frontiers in behavioral neuroscience, 19, 1524722. https://doi.org/10.3389/fnbeh.2025.1524722
Harvey A. R. (2023). Injury, illness, and emotion: A review of the motivational continuum from trauma through recovery from an ecological perspective. Brain, behavior, & immunity - health, 27, 100586. https://doi.org/10.1016/j.bbih.2022.100586
Helmich, M. A., Schreuder, M. J., Bringmann, L. F., Riese, H., Snippe, E., & Smit, A. C. (2024). Slow down and be critical before using early warning signals in psychopathology. Nature Reviews Psychology, 1-14.
Hermans, E. J., Hendler, T., & Kalisch, R. (2025). Building Resilience: The Stress Response as a Driving Force for Neuroplasticity and Adaptation. Biological psychiatry, 97(4), 330–338. https://doi.org/10.1016/j.biopsych.2024.10.016
Huong, C., Bernstein, E. E., Curtiss, J. E., Kolar, D. R., & Brown, D. M. (2024). Network approaches for physical activity and mental health research. Sport, Exercise, and Performance Psychology.
Ibáñez, A., Duran-Aniotz, C., Migeot, J., Báez, S., Fittipaldi, S., Coronel-Oliveros, C., Eyre, H. A., Udeh-Momoh, C., Zetterberg, H., Alladi, S., Sandi, C., Robertson, I. H., Franzen, S., Farombi, T., Montalvo Ortiz, J. L., Seshadri, S., Court, F., Valdes-Sosa, P., Xu, J., Yu, C., … Santamaría-García, H. (2025). Computational whole-body-exposome models for global precision brain health. Nature communications, 16(1), 11078. https://doi.org/10.1038/s41467-025-67448-3
Iovoli, F., Hall, M., Nenadic, I., Straube, B., Alexander, N., Jamalabadi, H., Jansen, A., Stein, F., Brosch, K., Thomas-Odenthal, F., Usemann, P., Teutenberg, L., Wroblewski, A., Pfarr, J., Thiel, K., Flinkenflügel, K., Meinert, S., Grotegerd, D., Hahn, T., Goltermann, J., … Rubel, J. A. (2024). Exploring the complex interrelation between depressive symptoms, risk, and protective factors: A comprehensive network approach. Journal of affective disorders, 355, 12–21. https://doi.org/10.1016/j.jad.2024.03.119
Jinich-Diamant, A., Albinni, B., Fishbein, J. N., Jacobson, E., Abraira, V. E., Hong, S., Korgan, A. C., Mazzieri, A. M., & Case, L. (2025). MASSAG Model: Towards an Integrative Neuroscience Framework Linking Emotional Trauma, Pain, and Mechanisms of Force-Based Manipulations. Neuroscience and biobehavioral reviews, 106517. Advance online publication. https://doi.org/10.1016/j.neubiorev.2025.106517
Kapos, F. P., Craig, K. D., Anderson, S. R., Bernardes, S. F., Hirsh, A. T., Karos, K., Keogh, E., Reynolds Losin, E. A., McParland, J. L., Moore, D. J., & Ashton-James, C. E. (2024). Social Determinants and Consequences of Pain: Toward Multilevel, Intersectional, and Life Course Perspectives. The journal of pain, 25(10), 104608. https://doi.org/10.1016/j.jpain.2024.104608
Keever, T. (2025). The Whole Well-Being Model: A Layered Framework for Thriving People, Systems, and Planet. Global advances in integrative medicine and health, 14, 27536130251364869. https://doi.org/10.1177/27536130251364869
Kenzie, E. S., Parks, E. L., Bigler, E. D., Lim, M. M., Chesnutt, J. C., & Wakeland, W. (2017). Concussion As a Multi-Scale Complex System: An Interdisciplinary Synthesis of Current Knowledge. Frontiers in neurology, 8, 513. https://doi.org/10.3389/fneur.2017.00513
Kenzie, E. S., Parks, E. L., Bigler, E. D., Wright, D. W., Lim, M. M., Chesnutt, J. C., Hawryluk, G. W. J., Gordon, W., & Wakeland, W. (2018). The Dynamics of Concussion: Mapping Pathophysiology, Persistence, and Recovery With Causal-Loop Diagramming. Frontiers in neurology, 9, 203. https://doi.org/10.3389/fneur.2018.00203
Kerry, R., Young, K. J., Evans, D. W., Lee, E., Georgopoulos, V., Meakins, A., McCarthy, C., Cook, C., Ridehalgh, C., Vogel, S., Banton, A., Bergström, C., Mazzieri, A. M., Mourad, F., & Hutting, N. (2024). A modern way to teach and practice manual therapy. Chiropractic & manual therapies, 32(1), 17. https://doi.org/10.1186/s12998-024-00537-0
Keter, D. L., Bialosky, J. E., Brochetti, K., Courtney, C. A., Funabashi, M., Karas, S., Learman, K., & Cook, C. E. (2025). The mechanisms of manual therapy: A living review of systematic, narrative, and scoping reviews. PloS one, 20(3), e0319586. https://doi.org/10.1371/journal.pone.0319586
Kok, A. A. L., Huisman, M., Giltay, E. J., & Lunansky, G. (2025). Adopting a complex systems approach to functional ageing: bridging the gap between gerontological theory and empirical research. The lancet. Healthy longevity, 6(3), 100673. https://doi.org/10.1016/j.lanhl.2024.100673
Langevin, H. M. (2024). Health and Well-Being: Distinct and Intertwined Concepts. Medical care, 62(12 Suppl 1), S13–S14. https://doi.org/10.1097/MLR.0000000000002061
Langevin, H. M., Weber, W., & Chen, W. (2024). Integrated multicomponent interventions to support healthy aging of the whole person. Aging cell, 23(1), e14001. https://doi.org/10.1111/acel.14001
Lee, K. H., & Lee, C. E. (2025). The evolving landscape of health and social care integration: in search of a unifying theory. Frontiers in medicine, 12, 1464699. https://doi.org/10.3389/fmed.2025.1464699
Lei, D., & Djedovic, A. P. A. (2025). The Synergistic Mind-Body Hypothesis: A Daoist Approach to Consciousness from the Perspective of Traditional Chinese Medicine. Canadian Undergraduate Journal of Cognitive Science, 8.
Low, M., Moffatt, F. H., Kerry, R., & Nicholls, D. A. (2025). Physioethology: a post-humanist perspective on physiotherapy. Physiotherapy theory and practice, 1–19. Advance online publication. https://doi.org/10.1080/09593985.2025.2532572
Lunansky, G., Bonanno, G. A., Blanken, T. F., van Borkulo, C. D., Cramer, A. O. J., & Borsboom, D. (2025). Bouncing back from life's perturbations: Formalizing psychological resilience from a complex systems perspective. Psychological review, 132(6), 1396–1409. https://doi.org/10.1037/rev0000497
Lutke Schipholt, I. J., Coppieters, M. W., Scholten-Peeters, G. G. M., Hutchinson, M. R., & Klyne, D. M. (2025). Neuroimmune interactions in musculoskeletal conditions. An introduction for clinicians. Musculoskeletal science & practice, 81, 103469. Advance online publication. https://doi.org/10.1016/j.msksp.2025.103469
Martinez, V. M. L., Martins, M. D. S., Capra, F., Schuch, F. B., Wearick-Silva, L. E., & Feoli, A. M. P. (2024). The Impact of Physical Activity and Lifestyle on Mental Health: A Network Analysis. Journal of physical activity & health, 21(12), 1330–1340. https://doi.org/10.1123/jpah.2024-0198
McClean, Z. J., Pasanen, K., Lun, V., Charest, J., Herzog, W., Werthner, P., Black, A., Vleuten, R. V., Lacoste, E., & Jordan, M. J. (2024). A Biopsychosocial Model for Understanding Training Load, Fatigue, and Musculoskeletal Sport Injury in University Athletes: A Scoping Review. Journal of strength and conditioning research, 38(6), 1177–1188. https://doi.org/10.1519/JSC.0000000000004789
McParlin, Z., Cerritelli, F., Rossettini, G., Friston, K. J., & Esteves, J. E. (2022). Therapeutic Alliance as Active Inference: The Role of Therapeutic Touch and Biobehavioural Synchrony in Musculoskeletal Care. Frontiers in behavioral neuroscience, 16, 897247. https://doi.org/10.3389/fnbeh.2022.897247
McSwan, J., Panwar, C. E., & Mobasheri, A. (2025). Looking Inwards: The Role of Self-Care, Self-Management and Self-Healing in Musculoskeletal Pain. Musculoskeletal care, 23(3), e70169. https://doi.org/10.1002/msc.70169
Mickle, A. M., Tanner, J. J., Olowofela, B., Wu, S., Garvan, C., Lai, S., Addison, A., Przkora, R., Edberg, J. C., Staud, R., Redden, D., Goodin, B. R., Price, C. C., Fillingim, R. B., & Sibille, K. T. (2023). Elucidating individual differences in chronic pain and whole person health with allostatic load biomarkers. Brain, behavior, & immunity - health, 33, 100682. https://doi.org/10.1016/j.bbih.2023.100682
Minelli, A., Bottaccioli, A. G., & Bottaccioli, F. (2025). Psyche and Life: Allostasis between the Predictive brain-mind system and Traditional Chinese Medicine. PNEI review: rivista della Società Italiana di Psiconeuroendocrinoimmunologia: 1, 2025, 1-14.
Montano, M., Oursler, K. K., & Marconi, V. C. (2024). Healthy aging: Linking causal mechanisms with holistic outcomes. Aging cell, 23(1), e14065. https://doi.org/10.1111/acel.14065
Nadinda, P. G., van Laarhoven, A. I. M., Van den Bergh, O., Vlaeyen, J. W. S., Peters, M. L., & Evers, A. W. M. (2024). Expectancies and avoidance: Towards an integrated model of chronic somatic symptoms. Neuroscience and biobehavioral reviews, 164, 105808. https://doi.org/10.1016/j.neubiorev.2024.105808
Nesi, J., Benites, M., & Schedler, F. B. (2025). Enactivism: A contemporary perspective of a reconceptualization of osteopathy. Advances in Integrative Medicine, 12(3), 100416.
Nielsen, K., & Faulkner, J. (2025). Evaluating the complex systems approach to persisting post-concussion symptoms. Theory & Psychology, 35(1), 17-39.
Nijs, J., Malfliet, A., Roose, E., Lahousse, A., Van Bogaert, W., Johansson, E., Runge, N., Goossens, Z., Labie, C., Bilterys, T., Van Campenhout, J., Polli, A., Wyns, A., Hendrix, J., Xiong, H. Y., Ahmed, I., De Baets, L., & Huysmans, E. (2024). Personalized Multimodal Lifestyle Intervention as the Best-Evidenced Treatment for Chronic Pain: State-of-the-Art Clinical Perspective. Journal of clinical medicine, 13(3), 644. https://doi.org/10.3390/jcm13030644
Núñez-Cortés, R., Salazar-Méndez, J., & Nijs, J. (2025). Physical Activity as a Central Pillar of Lifestyle Modification in the Management of Chronic Musculoskeletal Pain: A Narrative Review. Journal of Functional Morphology and Kinesiology, 10(2), 183. https://doi.org/10.3390/jfmk10020183
Oikkonen, V., Helosvuori, E., Ganesh, A., & Rokkonen, L. A. (2025). Entangled Illnesses: Embodied Experiences of Managing Multimorbidity. Sociology of health & illness, 47(2), e70006. https://doi.org/10.1111/1467-9566.70006
Ozawa De Silva, C., & Ozawa-De Silva, B. R. (2011). Mind/body theory and practice in Tibetan medicine and Buddhism. Body & Society, 17(1), 95-119.
Packheiser, J., Hartmann, H., Fredriksen, K., Gazzola, V., Keysers, C., & Michon, F. (2024). A systematic review and multivariate meta-analysis of the physical and mental health benefits of touch interventions. Nature human behaviour, 8(6), 1088–1107. https://doi.org/10.1038/s41562-024-01841-8
Pessoa, L. (2025). Beyond networks: Toward adaptive models of biological complexity. Physics of life reviews, 56, 67–81. Advance online publication. https://doi.org/10.1016/j.plrev.2025.11.007
Pitcher, M. H., Edwards, E., Langevin, H. M., Rusch, H. L., & Shurtleff, D. (2023). Complementary and integrative health therapies in whole person resilience research. Stress and health : journal of the International Society for the Investigation of Stress, 39(S1), 55–61. https://doi.org/10.1002/smi.3276
Pollak, T., Levin, M., Bhat, A., Butler, M., Berlot, R., & Edwards, M. Have you tried switching it off and on again? Mechanisms and therapeutic prospects of resetting homeostatic set points in medicine and neuropsychiatry.
Quinlan, E. B., Baumgartner, J., Chen, W. G., Weber, W., Horgusluoglu, E., & Edwards, E. (2024). Promoting salutogenic pathways to health through complementary and integrative health approaches. Frontiers in psychology, 15, 1473735. https://doi.org/10.3389/fpsyg.2024.1473735
Rabey, M., & Moloney, N. (2022). "I Don't Know Why I've Got this Pain!" Allostasis as a Possible Explanatory Model. Physical therapy, 102(5), pzac017 https://doi.org/10.1093/ptj/pzac017
Rojas-Valverde, D., Herrera-González, E., & Bonilla, D. A. (2025). Sports injuries as reversible involution: a novel approach to rehabilitation and readaptation. Frontiers in sports and active living, 7, 1519404. https://doi.org/10.3389/fspor.2025.1519404
Santamaría-García, H., Migeot, J., Medel, V., Hazelton, J. L., Teckentrup, V., Romero-Ortuno, R., Piguet, O., Lawor, B., Northoff, G., & Ibanez, A. (2025). Allostatic Interoceptive Overload Across Psychiatric and Neurological Conditions. Biological psychiatry, 97(1), 28–40. https://doi.org/10.1016/j.biopsych.2024.06.024
Scheffer, M., Bockting, C. L., Borsboom, D., Cools, R., Delecroix, C., Hartmann, J. A., Kendler, K. S., van de Leemput, I., van der Maas, H. L. J., van Nes, E., Mattson, M., McGorry, P. D., & Nelson, B. (2024). A Dynamical Systems View of Psychiatric Disorders-Theory: A Review. JAMA psychiatry, 81(6), 618–623. https://doi.org/10.1001/jamapsychiatry.2024.0215
Scheffer, M., Bockting, C. L., Borsboom, D., Cools, R., Delecroix, C., Hartmann, J. A., Kendler, K. S., van de Leemput, I., van der Maas, H. L. J., van Nes, E., Mattson, M., McGorry, P. D., & Nelson, B. (2024). A Dynamical Systems View of Psychiatric Disorders-Practical Implications: A Review. JAMA psychiatry, 81(6), 624–630. https://doi.org/10.1001/jamapsychiatry.2024.0228
Schüler, J., Heino, M. T. J., Balagué, N., Chater, A. M., Gruber, M., Kanning, M., Keim, D., Mier, D., Moreno-Villanueva, M., Nussbeck, F. W., Pruessner, J., Shafie, T., Schwenk, M., & Bieleke, M. (2025). A complex systems view on physical activity with actionable insights for behaviour change. Nature human behaviour, 9(9), 1793–1801. https://doi.org/10.1038/s41562-025-02279-2
Sedley, W., Kumar, S., Jones, S., Levy, A., Friston, K., Griffiths, T., & Goldsmith, P. (2024). Migraine as an allostatic reset triggered by unresolved interoceptive prediction errors. Neuroscience and biobehavioral reviews, 157, 105536. https://doi.org/10.1016/j.neubiorev.2024.105536
Shepherd, M. H., McDevitt, A., Keter, D., Albers, N., Clewley, D., & Cook, C. (2025). The person-centered hypothesis framework: Advancing clinical reasoning in musculoskeletal pain management. Musculoskeletal science & practice, 80, 103395. https://doi.org/10.1016/j.msksp.2025.103395
Slater, H., & Briggs, A. M. (2024). Strengthening the pain care ecosystem to support equitable, person-centered, high-value musculoskeletal pain care. Pain, 165(11S), S92–S107. https://doi.org/10.1097/j.pain.0000000000003373
Strahl, A., Maehder, K., Toussaint, A., Hasenbank, N., Schramm, C., Lohse, A. W., ... & Löwe, B. (2025). Mapping the Network of Persistent Somatic Symptoms Across Diseases: A Longitudinal Analysis from the SOMACROSS Research Unit. medRxiv, 2025-09.
Sturmberg, J. P., & Martin, C. M. (2024). From theory to practice: The pragmatic value of applying systems thinking and complexity sciences in healthcare. Journal of evaluation in clinical practice, 30(2), 149–152. https://doi.org/10.1111/jep.13979
Sturmberg, J. P., & Mercuri, M. (2025). Every problem is embedded in a greater whole. Journal of evaluation in clinical practice, 31(1), e14139. https://doi.org/10.1111/jep.14139
Tabor, A., & Constant, A. (2023). Lifeworlds in pain: a principled method for investigation and intervention. Neuroscience of consciousness, 2023(2), niad021. https://doi.org/10.1093/nc/niad021
Tanner, J. J., Mickle, A., Holmes, U., 3rd, Addison, B., Rangel, K., Garvan, C., Staud, R., Lai, S., Redden, D., Goodin, B. R., Price, C. C., Fillingim, R. B., & Sibille, K. T. (2025). More than chronic pain: behavioural and psychosocial protective factors predict lower brain age in adults with/at risk of knee osteoarthritis over two years. Brain communications, 7(5), fcaf344. https://doi.org/10.1093/braincomms/fcaf344
Theriault, J. E., Katsumi, Y., Reimann, H. M., Zhang, J., Deming, P., Dickerson, B. C., Quigley, K. S., & Barrett, L. F. (2025). It's not the thought that counts: Allostasis at the core of brain function. Neuron, S0896-6273(25)00716-0. Advance online publication. https://doi.org/10.1016/j.neuron.2025.09.028
Topolski, S. (2009). Understanding health from a complex systems perspective. Journal of evaluation in clinical practice, 15(4), 749–754. https://doi.org/10.1111/j.1365-2753.2009.01227.x
Turvill, A., Maratos, F., & Sheffield, D. (2026). Assessing the Impact of Interdisciplinary Multimodal Pain Treatment on Health-Related Quality of Life in Chronic Pain: A Systematic Review and Meta-Analyses. European journal of pain (London, England), 30(1), e70176. https://doi.org/10.1002/ejp.70176
Uleman, J. F., Stronks, K., Rutter, H., Arah, O. A., & Rod, N. H. (2024). Mapping complex public health problems with causal loop diagrams. International journal of epidemiology, 53(4), dyae091. https://doi.org/10.1093/ije/dyae091
van der Greef, J., van Wietmarschen, H., Schroën, Y., Babouraj, N., & Trousselard, M. (2015). Systematic approaches to evaluation and integration of eastern and Western medical practices. Medical acupuncture, 27(5), 384-395.
Varangot-Reille, C., Pezzulo, G., & Thacker, M. (2024). The fear-avoidance model as an embodied prediction of threat. Cognitive, affective & behavioral neuroscience, 24(5), 781–792. https://doi.org/10.3758/s13415-024-01199-4
Vaz, D. V., Stilwell, P., Coninx, S., Low, M., & Liebenson, C. (2023). Affordance-based practice: An ecological-enactive approach to chronic musculoskeletal pain management. Brazilian journal of physical therapy, 27(5), 100554. https://doi.org/10.1016/j.bjpt.2023.100554
Verhagen, E., McGinley, P., & McKay, C. D. (2025). Beyond tame solutions: a new paradigm for injury prevention in sports. BMJ open sport & exercise medicine, 11(2), e002478. https://doi.org/10.1136/bmjsem-2025-002478
Wayne, P. M., Ahn, A., Clark, J., Irwin, M. R., Kong, J., Lavretsky, H., Li, F., Manor, B., Mehling, W., Oh, B., Seitz, D., Tawakol, A., Tsang, W. W. N., Wang, C., Yeung, A., & Yeh, G. Y. (2025). The Science of Tai Chi and Qigong as Whole Person Health-Part I: Rationale and State of the Science. Journal of integrative and complementary medicine, 31(6), 499–520. https://doi.org/10.1089/jicm.2024.0957
Wang, S. B., Blanken, T. F., van der Maas, H. L. J., & Borsboom, D. (2025). Path Asymmetry in Complex Dynamic Systems of Psychopathology. JAMA psychiatry, 10.1001/jamapsychiatry.2025.3147. Advance online publication. https://doi.org/10.1001/jamapsychiatry.2025.3147
Zegarra-Parodi, R., D'Alessandro, G., Baroni, F., Swidrovich, J., Mehl-Madrona, L., Gordon, T., Ciullo, L., Castel, E., & Lunghi, C. (2024). Epistemological Flexibility in Person-Centered Care: The Cynefin Framework for (Re)Integrating Indigenous Body Representations in Manual Therapy. Healthcare (Basel, Switzerland), 12(11), 1149. https://doi.org/10.3390/healthcare12111149