Massage Therapy and Postoperative Care
/The use of massage therapy has been shown to improve outcomes in post-operative patients.
One recent paper published in the journal PM&R, looked at the use of fascial manipulation following total hip arthroplasty (Busato et al. 2016). In this study 2 treatment sessions were are able to significantly improve functional outcomes in patients when used in addition to usual treatment.
Another recent study published in The Journal of Knee Surgery looked at the effect that soft-tissue treatments with hand-held instruments have on post-surgical knee stiffness (Chunghtai et al. 2016). In the study soft-tissue treatments was shown to improve knee flexion deficits by 35° and knee flexion contractures by 12° in a small cohort of individuals who had failed to respond to traditional rehabilitation and manipulation under anesthesia.
So like I have posted in a number of posts before (here, here, here, here) massage therapy is simple to carry out, economical, and has very few side effects. In this post I will highlight a few ways to massage therapy may be used to improve outcomes in postoperative patients.
What is the the rationale for using massage therapy?
The body of knowledge to support the use of massage therapy continues to grow, understanding the basic science behind what we do and the guiding principles of adaptability enable us to apply this work to a number of pathological conditions.
Postoperative Pain Management
The responses to massage therapy are complex and multifactorial - physiological and psychological factors interplay in a complex manner. Research has looked at neuroimmune responses at both the peripheral and central levels elicited by massage therapy treatments.
In short - Massage has a modulatory affect on peripheral and central processes via mechanoreceptors. Input from large sensory neurons activate spinal cord interneurons that prevents the spinal cord from amplifying the nociceptive signal. This anti-nociceptive effect of massage therapy can help ease discomfort in post surgical patients (Bishop et al. 2015, Vigotsky et al. 2015).
Postoperative Fibrosis
Additionally, massage therapy may improve healing after trauma and in some cases ameliorate the degree of postoperative fibrosis.
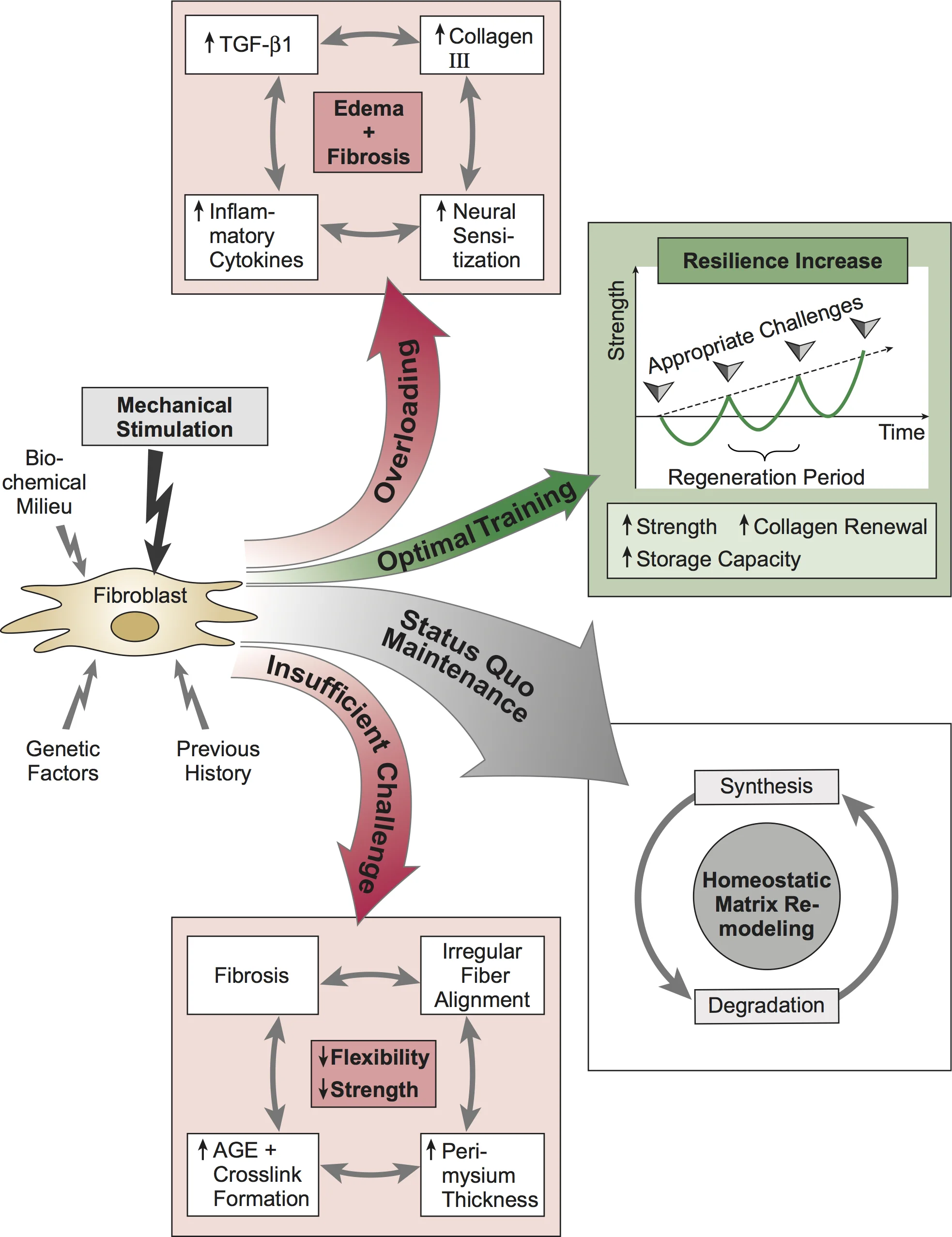
Mechanotherapy - “any intervention that introduces mechanical forces with the goal of altering molecular pathways and inducing a cellular response that enhances tissue growth, modeling, remodeling, or repair.”
Fibrosis is a potential complication of surgery or trauma, it is characterized by the production of excessive fibrous scar tissue, which may result in decreased movement. Understanding the cellular effectors and signaling pathways that drives the accumulation of fibrotic deposition, helps therapists optimize treatment protocols for patients suffering from post-surgical fibrosis and guide specific prophylactic treatments.
TGF-Β1 PLAYS A ROLE IN TISSUE REMODELING, AS A THERAPEUTIC INTERVENTION MASSAGE THERAPY HAS THE POTENTIAL TO ATTENUATE TGF-Β1 INDUCED FIBROBLAST TO MYOFIBROBLAST TRANSFORMATION
DAVIS'S LAW, ATTRIBUTION: WWW.FASCIALNET.COM
In the normal wound healing response, the cascade of biological responses is tightly regulated. Fibrotic development is characterized by a lack of apoptosis in the proinflammatory phase, resulting in an imbalance between synthesis and degradation. Persistent transforming growth factor-β (TGF-β) secretion and downstream responses are thought to contribute to a sustained inflammatory response (Cheuy et al. 2017).
Manual mobilization is a promising strategy that is used to attenuate adhesion formation and minimize the loss of mobility due to fibrosis. Recent studies have looked at the effect of modeled massage therapy on tissue levels of TGF-β1 (Bove et al. 2016). In this study it was demonstrated manual therapy attenuated the increased fibrosis and tissue levels of TGF-β1, this may play a role in disease development by reducing the contractile activity of myofibroblasts.
In short - The rationale is that the application of appropriate shear force and pressure impart a mechanical stimulus that may attenuate tissue levels of TGF-β1.
Summary Points
The use of prophylactic massage therapy may help patients manage postoperative pain. It may also affect the development of fibrosis by mediating differential cytokine production.
The next step for researchers is to look into what sort of dosage and duration would be needed to optimize the effects of this non-pharmacological approach.
More to Explore
Related Links
• Traumatic Muscle Fibrosis: From pathway to prevention
• Massage Therapy and Compartment Syndrome
• The Role of Massage in Scar Management
• Research on Massage and Cancer
• Sports Massage - The Science is Emerging
• Massage Therapy and Dupuytren's Disease
Research Links
Ali, A., Rosenberger, L., Weiss, T.R., Milak, C., Perlman, A.I. (2017). Massage Therapy and Quality of Life in Osteoarthritis of the Knee: A Qualitative Study. Pain Med.
https://www.ncbi.nlm.nih.gov/pubmed/27590465
Alvira-Lechuz, J., Espiau, M.R., Alvira-Lechuz, E. (2017). Treatment of the scar after arthroscopic surgery on a knee. J Bodyw Mov Ther.
https://www.ncbi.nlm.nih.gov/pubmed/28532876
Begovic, H., Zhou, G., Schuster, S., & Zheng, Y. (2016). The neuromotor effects of transverse friction massage. Manual Therapy.
https://www.ncbi.nlm.nih.gov/pubmed/27497646
Berrueta, L., Muskaj, I., Olenich, S., Butler, T., Badger, G. J., Colas, R. A., . . . Langevin, H. M. (2016). Stretching Impacts Inflammation Resolution in Connective Tissue. Journal of Cellular Physiology.
http://www.ncbi.nlm.nih.gov/pubmed/26588184
Best, T., Gharaibeh, B., & Huard, J. (2013). Stem cells, angiogenesis and muscle healing: A potential role in massage therapies? British Journal of Sports Medicine.
https://www.ncbi.nlm.nih.gov/pubmed/23197410
Bijlard, E., Uiterwaal, L., ... Huygen, F.J. (2017). A Systematic Review on the Prevalence, Etiology, and Pathophysiology of Intrinsic Pain in Dermal Scar Tissue. Pain Physician.
https://www.ncbi.nlm.nih.gov/pubmed/28158149 (OPEN ACCESS)
Bishop, M. D., Torres-Cueco, R., Gay, C. W., Lluch-Girbés, E., Beneciuk, J. M., & Bialosky, J. E. (2015). What effect can manual therapy have on a patient's pain experience? Pain Management.
https://www.ncbi.nlm.nih.gov/pubmed/26401979 (OPEN ACCESS)
Bochaton-Piallat, M., Gabbiani, G., & Hinz, B. (2016). The myofibroblast in wound healing and fibrosis: Answered and unanswered questions. F1000Research.
https://www.ncbi.nlm.nih.gov/pubmed/27158462 (OPEN ACCESS)
Bove, G., & Chapelle, S. (2012). Visceral mobilization can lyse and prevent peritoneal adhesions in a rat model. Journal of Bodywork and Movement Therapies.
http://www.ncbi.nlm.nih.gov/pubmed/22196431
Bove, G., Harris, M., Zhao, H., & Barbe, M. (2016). Manual therapy as an effective treatment for fibrosis in a rat model of upper extremity overuse injury. Journal of the Neurological Sciences.
http://www.ncbi.nlm.nih.gov/pubmed/26810536 (OPEN ACCESS)
Busato, M., Quagliati, C.,...Stecco, A. (2016). Fascial Manipulation Associated With Standard Care Compared to Only Standard Postsurgical Care for Total Hip Arthroplasty: A Randomized Controlled Trial. PM R.
https://www.ncbi.nlm.nih.gov/pubmed/27210234
Cezar, C.A., Roche, E.T., Vandenburgh, H.H., Duda, G.N., Walsh, C.J., Mooney, D.J. (2016). Biologic-free mechanically induced muscle regeneration. Proc Natl Acad Sci U S A.
https://www.ncbi.nlm.nih.gov/pubmed/26811474 (OPEN ACCESS)
Cheatham, S.W., Lee, M., Cain, M., Baker, R. (2016). The efficacy of instrument assisted soft tissue mobilization: a systematic review. J Can Chiropr Assoc.
https://www.ncbi.nlm.nih.gov/pubmed/27713575 (OPEN ACCESS)
Chaudhry, H., Bukiet, B., Ji, Z., Stecco, A., Findley, T.W. (2014). Deformations experienced in the human skin, adipose tissue, and fascia in osteopathic manipulative medicine. J Am Osteopath Assoc.
https://www.ncbi.nlm.nih.gov/pubmed/25288713
Chaitow, L. (2016). New evidence of a dynamic fascial maintenance and self-repair process. Journal of Bodywork and Movement Therapies.
https://www.ncbi.nlm.nih.gov/pubmed/27814847
Chaitow, L. (2016). Dosage and manual therapies – Can we translate science into practice? Journal of Bodywork and Movement Therapies.
https://www.ncbi.nlm.nih.gov/pubmed/27210835
Chapman, C.R., Vierck, C.J. (2017). The Transition of Acute Postoperative Pain to Chronic Pain: An Integrative Overview of Research on Mechanisms. J Pain.
https://www.ncbi.nlm.nih.gov/pubmed/27908839
Cheuy, V.A., Foran, J.R., Paxton, R.J., Bade, M.J., Zeni, J.A., Stevens-Lapsley, J.E. (2017). Arthrofibrosis Associated With Total Knee Arthroplasty. J Arthroplasty.
https://www.ncbi.nlm.nih.gov/pubmed/28285897
Cholok, D., Lee, E., ... Levi, B. (2017). Traumatic muscle fibrosis: From pathway to prevention. J Trauma Acute Care Surg.
https://www.ncbi.nlm.nih.gov/pubmed/27787441
Chughtai, M., Mont, M.A., ..., Bhave, A. (2016). A Novel, Nonoperative Treatment Demonstrates Success for Stiff Total Knee Arthroplasty after Failure of Conventional Therapy. J Knee Surg.
https://www.ncbi.nlm.nih.gov/pubmed/26713596
Comesaña, A. C., Vicente, M. D., Ferreira, T. D., Ma Del Mar Pérez-La Fuente Varela, Quintáns, M. M., & Pilat, A. (2017). Effect of myofascial induction therapy on post-c-section scars of more than one and a half years old. Pilot study. Journal of Bodywork and Movement Therapies.
https://www.ncbi.nlm.nih.gov/pubmed/28167179
Cook, C.E., Rhon, D.I., Lewis, B.D., George, S.Z. (2017). Post-operative opioid pain management patterns for patients who receive hip surgery.
https://www.ncbi.nlm.nih.gov/pubmed/28298221
Fisher, P., Zhao, Y., Rico, M., Massicotte, V., Wade, C., Litvin, J., . . . Barbe, M. (2015). Increased CCN2, substance P and tissue fibrosis are associated with sensorimotor declines in a rat model of repetitive overuse injury. Journal of Cell Communication and Signaling.
https://www.ncbi.nlm.nih.gov/pubmed/25617052 (OPEN ACCESS)
Gigliotti, D., Xu, M.C., Davidson, M.J., Macdonald, P.B., Leiter, J.R., Anderson, J.E. (2017). Fibrosis, low vascularity, and fewer slow fibers after rotator-cuff injury. Muscle Nerve.
https://www.ncbi.nlm.nih.gov/pubmed/2757128
Kai, F., Laklai, H., & Weaver, V. M. (2016). Force Matters: Biomechanical Regulation of Cell Invasion and Migration in Disease. Trends in Cell Biology.
https://www.ncbi.nlm.nih.gov/pubmed/27056543
Kalson, N.S., Borthwick, L.A., Mann, D.A. ...Krenn, V. (2016). International consensus on the definition and classification of fibrosis of the knee joint. Bone Joint J.
https://www.ncbi.nlm.nih.gov/pubmed/27803223
Kim, J., Sung, D.J., Lee, J. (2017). Therapeutic effectiveness of instrument-assisted soft tissue mobilization for soft tissue injury: mechanisms and practical application. J Exerc Rehabil.
https://www.ncbi.nlm.nih.gov/pubmed/28349028 (OPEN ACCESS)
Kemp, J., Moore, K., Fransen, M., Russell, T., Freke, M., Crossley, K.M. (2017). A pilot randomised clinical trial of physiotherapy (manual therapy, exercise, and education) for early-onset hip osteoarthritis post-hip arthroscopy. Pilot Feasibility Stud.
https://www.ncbi.nlm.nih.gov/pubmed/28694995
Kwan, P.O., Tredget, E.E. (2017). Biological Principles of Scar and Contracture. Hand Clin.
https://www.ncbi.nlm.nih.gov/pubmed/28363295
Laumonier, T., & Menetrey, J. (2016). Muscle injuries and strategies for improving their repair. Journal of Experimental Orthopaedics.
https://www.ncbi.nlm.nih.gov/pubmed/27447481 (OPEN ACCESS)
Loskotová, A., Loskotová, J., Suchanek, I., Brychta, P., Lipový, B. (2017). Myofascial-manual lymphatic drainage for burn trauma: a service evaluation. Br J Community Nurs.
https://www.ncbi.nlm.nih.gov/pubmed/28467220
Nanchahal, J., Hinz, B. (2016). Strategies to overcome the hurdles to treat fibrosis, a major unmet clinical need. Proc Natl Acad Sci U S A.
https://www.ncbi.nlm.nih.gov/pubmed/27342865 (OPEN ACCESS)
Noehren, B., Andersen, A., Hardy, P., Johnson, D. L., Ireland, M. L., Thompson, K. L., & Damon, B. (2016). Cellular and Morphological Alterations in the Vastus Lateralis Muscle as the Result of ACL Injury and Reconstruction. The Journal of Bone & Joint Surgery.
https://www.ncbi.nlm.nih.gov/pubmed/27655981
Nordez, A., Gross, R., Andrade, R., Le Sant, G., Freitas, S., Ellis, R., McNair, P.J., Hug, F. (2017). Non-Muscular Structures Can Limit the Maximal Joint Range of Motion during Stretching. Sports Med.
https://www.ncbi.nlm.nih.gov/pubmed/28255938
Parmar, S., Shyam, A., Sabnis, S., & Sancheti, P. (2011). The effect of isolytic contraction and passive manual stretching on pain and knee range of motion after hip surgery: A prospective, double-blinded, randomized study. Hong Kong Physiotherapy Journal.
http://www.sciencedirect.com/science/article/pii/S1013702511000054
Parravicini, G., Bergna, A., (2017). Biological effects of direct and indirect manipulation of the fascial system. Narrative review. Journal of Bodywork & Movement Therapies.
https://www.ncbi.nlm.nih.gov/pubmed/28532888
Pavan, P., Stecco, A., Stern, R., & Stecco, C. (2014). Painful Connections: Densification Versus Fibrosis of Fascia. Curr Pain Headache Rep Current Pain and Headache Reports.
http://www.ncbi.nlm.nih.gov/pubmed/25063495
Rand, E., Gellhorn, A.C. The Healing Cascade: Facilitating and Optimizing the System. Phys Med Rehabil Clin N Am.
https://www.ncbi.nlm.nih.gov/pubmed/27788901
Salamh, P., Cook, C., Reiman, M.P., Sheets, C. (2017). Treatment effectiveness and fidelity of manual therapy to the knee: A systematic review and meta-analysis. Musculoskeletal Care.
https://www.ncbi.nlm.nih.gov/pubmed/27860218
Sauber, R., Saborio, G., Nickel, B.M., Kivlan, B.R., Christoforetti, J.J. (2016). Pendulum Exercises After Hip Arthroscopy: A Video Technique. Arthrosc Tech.
https://www.ncbi.nlm.nih.gov/pubmed/27709055
Stecco, A., Stern, R., Fantoni, I., Caro, R., & Stecco, C. (2016). Fascial Disorders: Implications for Treatment. Pm&r.
http://www.ncbi.nlm.nih.gov/pubmed/26079868
Thompson, W. R., Scott, A., Loghmani, M. T., Ward, S. R., & Warden, S. J. (2016). Understanding Mechanobiology: Physical Therapists as a Force in Mechanotherapy and Musculoskeletal Regenerative Rehabilitation. Physical Therapy.
https://www.ncbi.nlm.nih.gov/pubmed/26637643 (OPEN ACCESS)
Vigotsky, A. D., & Bruhns, R. P. (2015). The Role of Descending Modulation in Manual Therapy and Its Analgesic Implications: A Narrative Review. Pain Research and Treatment.
https://www.ncbi.nlm.nih.gov/pubmed/26788367 (OPEN ACCESS)
Wasserman, J.B., Steele-Thornborrow, J.L., Yuen, J.S., Halkiotis, M., Riggins, E.M. (2016). Chronic caesarian section scar pain treated with fascial scar release techniques: A case series. J Bodyw Mov Ther.
https://www.ncbi.nlm.nih.gov/pubmed/27814873
Waters-Banker, C., Dupont-Versteegden, E. E., Kitzman, P. H., & Butterfield, T. A. (2014). Investigating the Mechanisms of Massage Efficacy: The Role of Mechanical Immunomodulation. Journal of Athletic Training.
https://www.ncbi.nlm.nih.gov/pubmed/24641083 (OPEN ACCESS)
Weppler, C.H., Magnusson, S.P. (2010). Increasing muscle extensibility: a matter of increasing length or modifying sensation? Phys Ther.
https://www.ncbi.nlm.nih.gov/pubmed/20075147
Wong, R., Geyer, S., Weninger, W., Guimberteau, J., & Wong, J. K. (2016). The dynamic anatomy and patterning of skin. Experimental Dermatology.
http://www.ncbi.nlm.nih.gov/pubmed/26284579
Wong, Y., Smith, R., & Koppenhaver, S. (2015). Soft Tissue Mobilization to Resolve Chronic Pain and Dysfunction Associated With Post-Operative Abdominal and Pelvic Adhesions: A Case Report. Journal of Orthopaedic & Sports Physical Therapy.
https://www.ncbi.nlm.nih.gov/pubmed/26471853
Wu, M., Chen, K., Chen, I., Huang, S. K., Tzeng, P., Yeh, M., . . . Chen, C. (2016). The Efficacy of Acupuncture in Post-Operative Pain Management: A Systematic Review and Meta-Analysis. PLOS ONE.
http://www.ncbi.nlm.nih.gov/pubmed/26959661